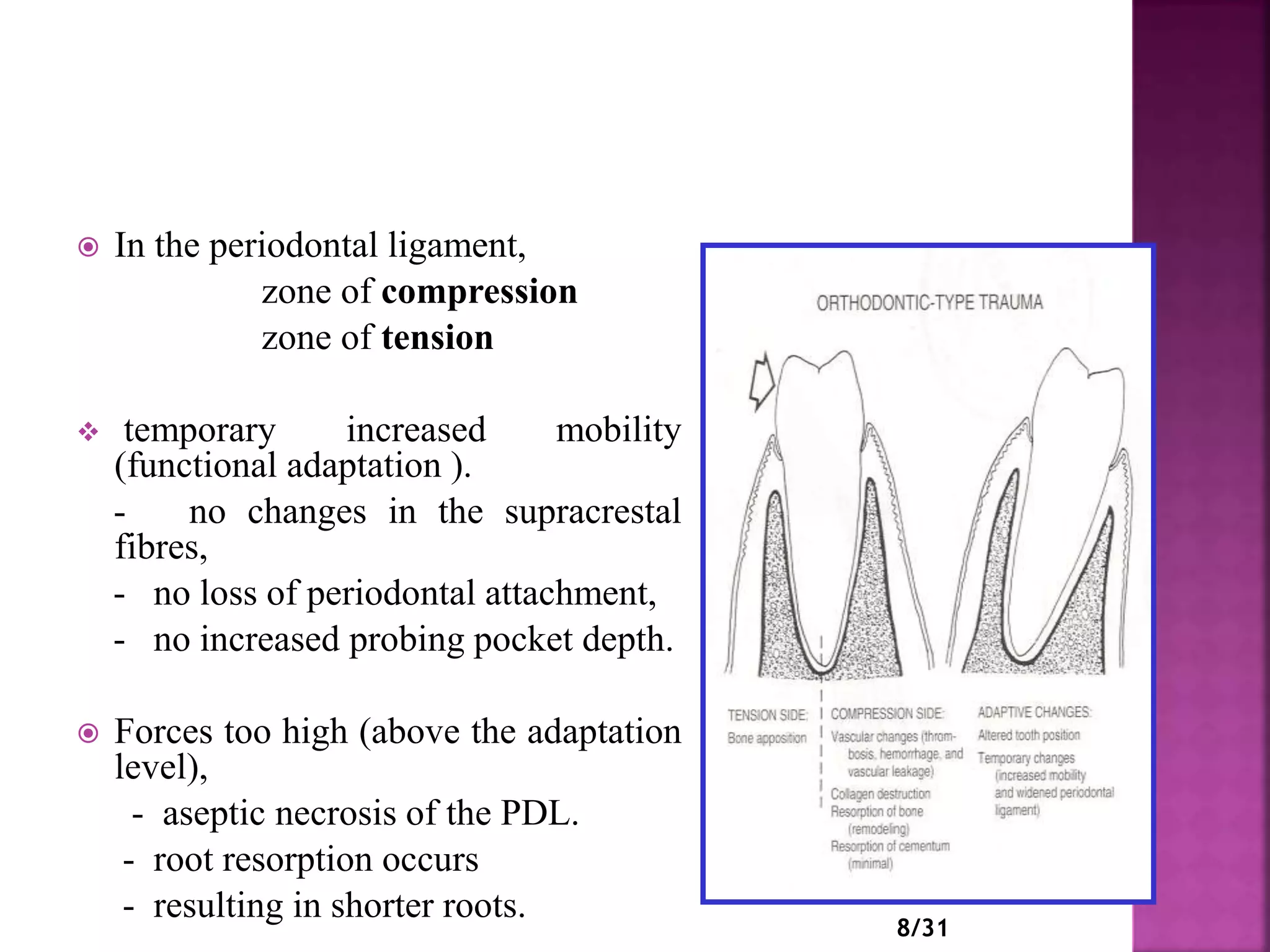
The document discusses trauma from occlusion (TFO), which occurs when excessive occlusal forces cause pathological changes in the periodontium. It outlines clinical features, diagnosis, and treatment approaches associated with TFO, emphasizing the impact of occlusal trauma on dental health and implant success. The document also reviews key concepts and theories, including those by Glickman and Waerhaug, regarding the relationship between occlusion, periodontal tissue response, and disease progression.