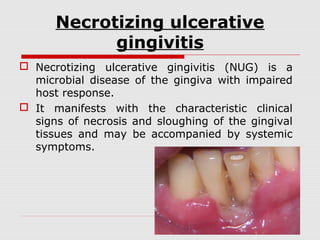
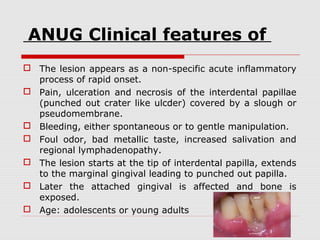
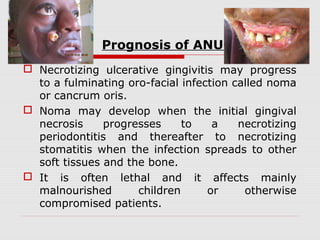
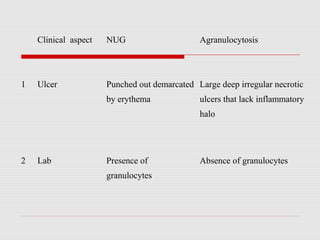
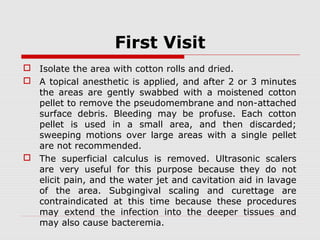
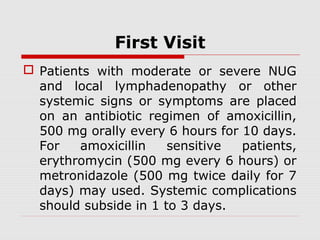
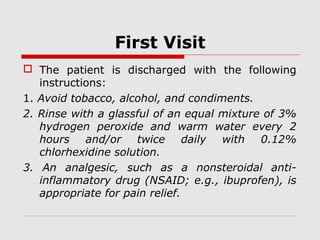
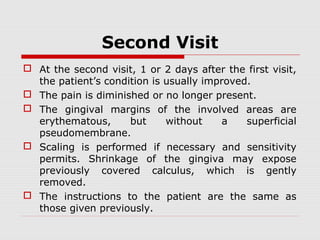
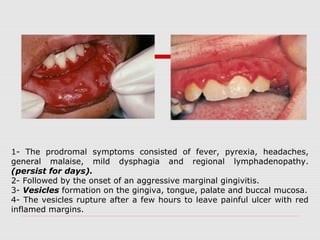
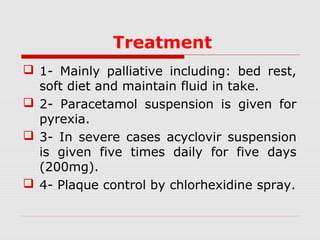
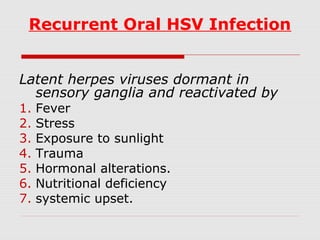
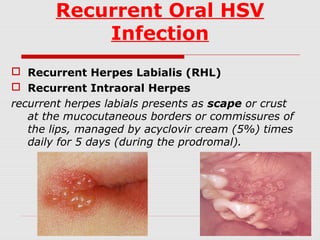
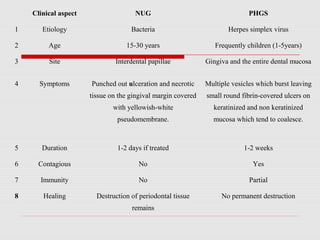
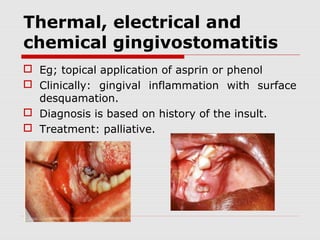
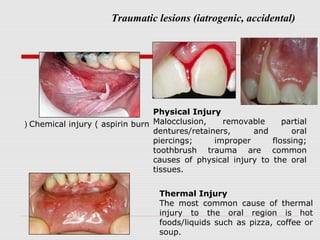
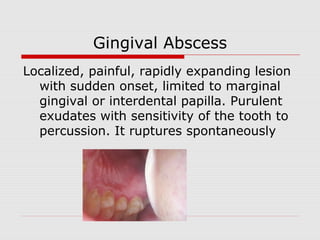
The document discusses various acute gingival conditions including necrotizing ulcerative gingivitis, acute herpetic gingivostomatitis, thermal/chemical gingivostomatitis, pericoronitis, and gingival abscess. It provides details on the etiology, clinical features, diagnosis, and treatment approaches for each condition. The conditions can cause pain, ulceration and necrosis of gingival tissues if left untreated.