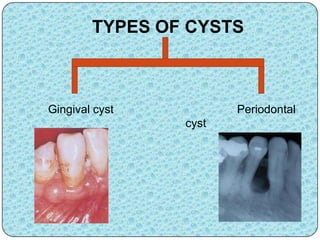
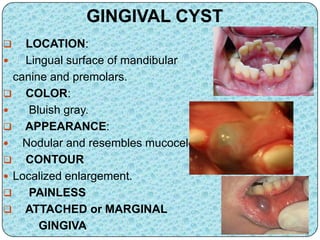
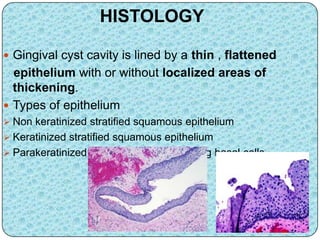
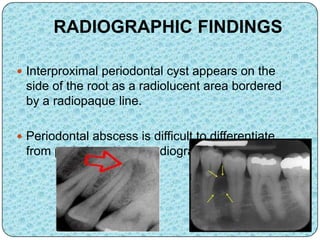
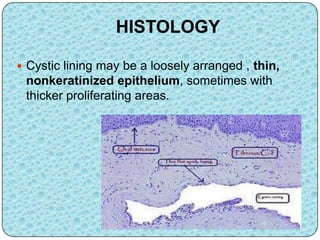
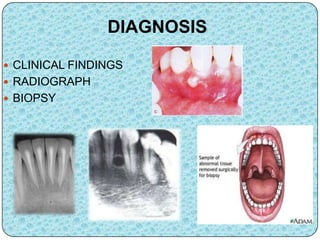
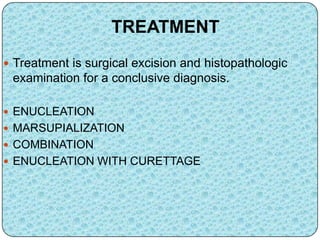
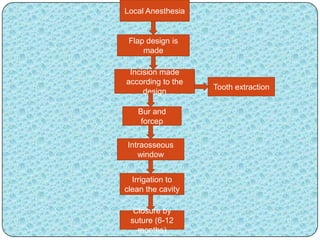
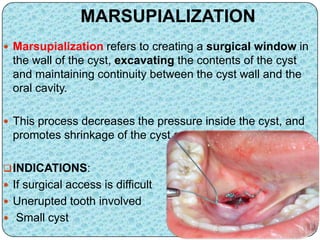
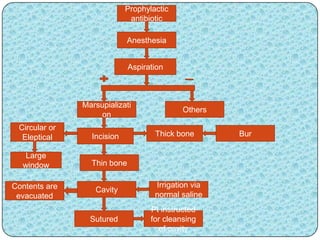
This document discusses cysts, specifically gingival and periodontal cysts. It defines a cyst as a pathological fluid-filled cavity lined by epithelium. Gingival cysts typically appear as bluish nodules on the gingiva near the mandibular canine and premolars. Periodontal cysts occur on lateral root surfaces and are derived from rests of Malassez. Diagnosis involves clinical and radiographic examination as well as biopsy. Treatment options include surgical excision through enucleation, marsupialization, or a combination approach.