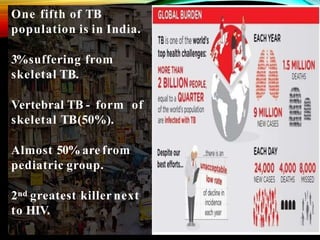
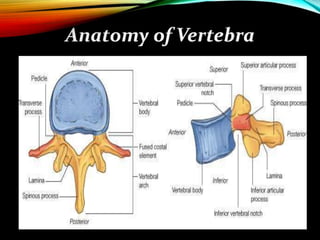
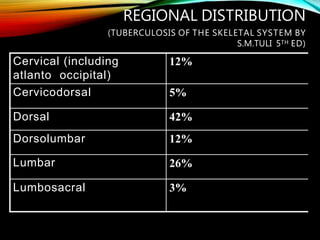
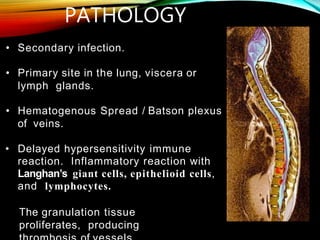
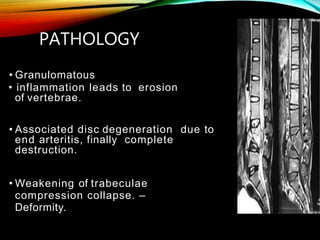
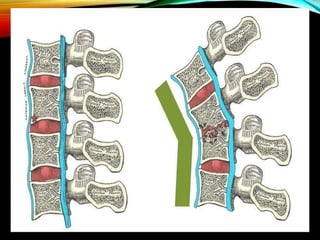
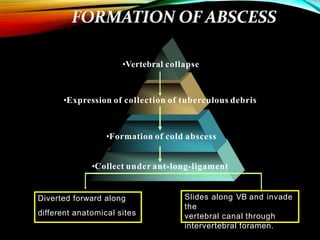
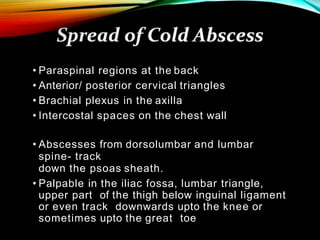
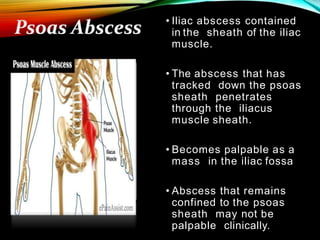
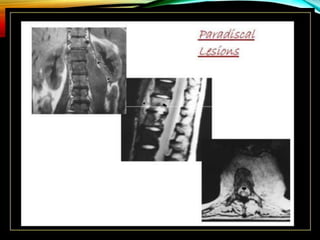
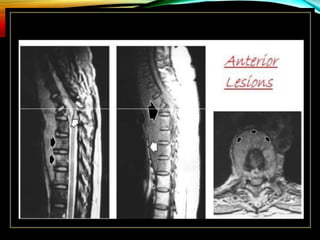
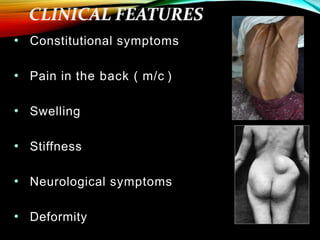
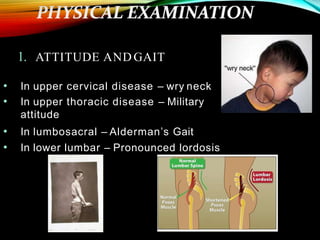
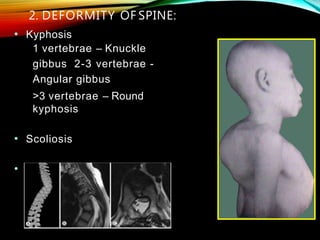
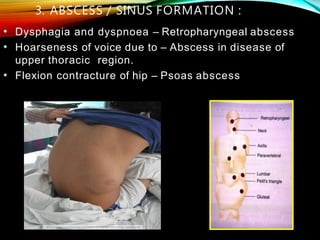
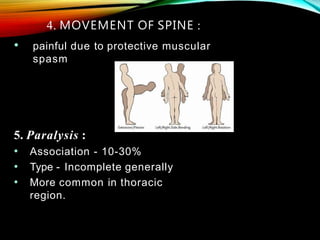
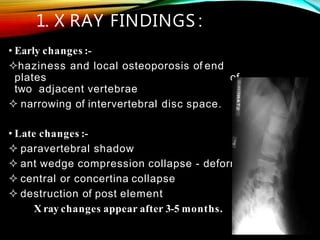
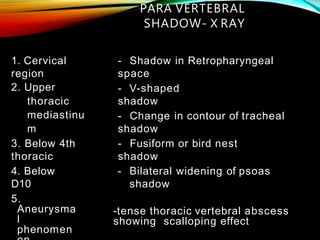
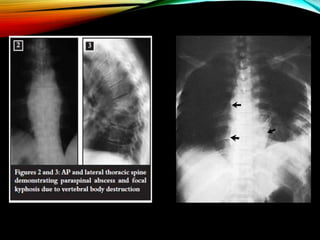
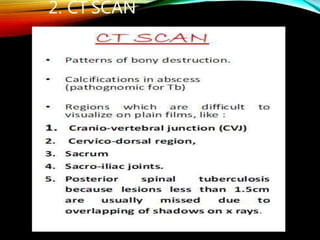
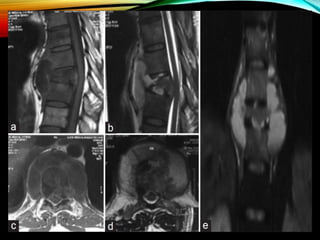
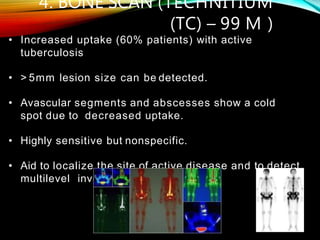
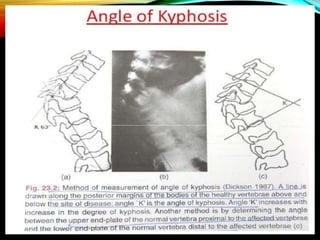
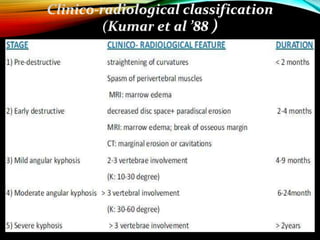
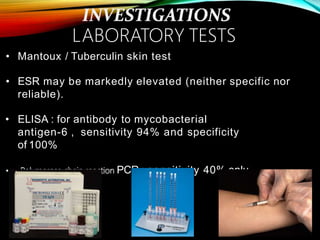
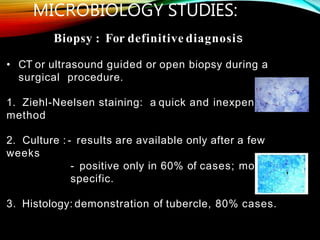
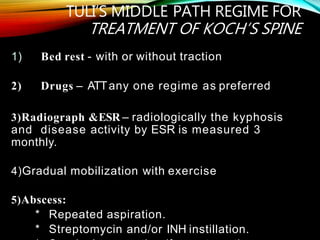
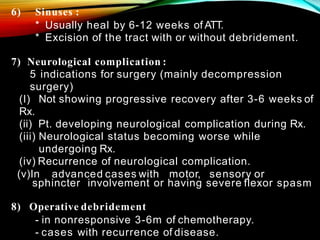
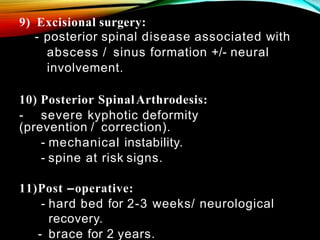
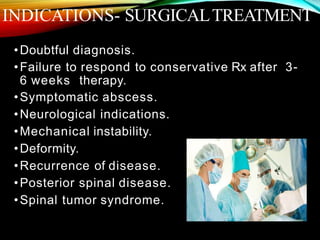
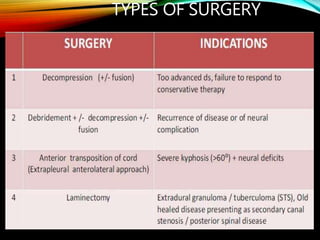
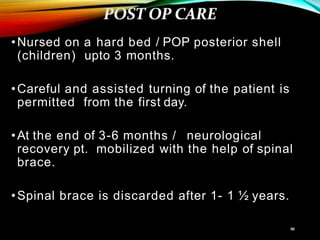
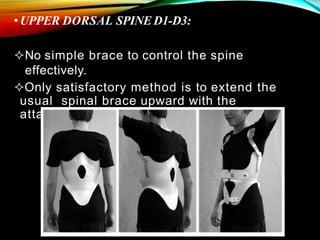
This document provides information on tuberculosis of the skeletal system (Potts disease). It discusses the history, epidemiology, pathogenesis, clinical presentation, investigations including imaging findings, microbiological studies, treatment including medical management and surgical options, as well as outcomes of skeletal tuberculosis. Key points include that India accounts for a large portion of global tuberculosis cases, it most commonly involves the thoracic spine, and treatment involves a combination of anti-tubercular medications and surgery in some cases to address complications or deformities.