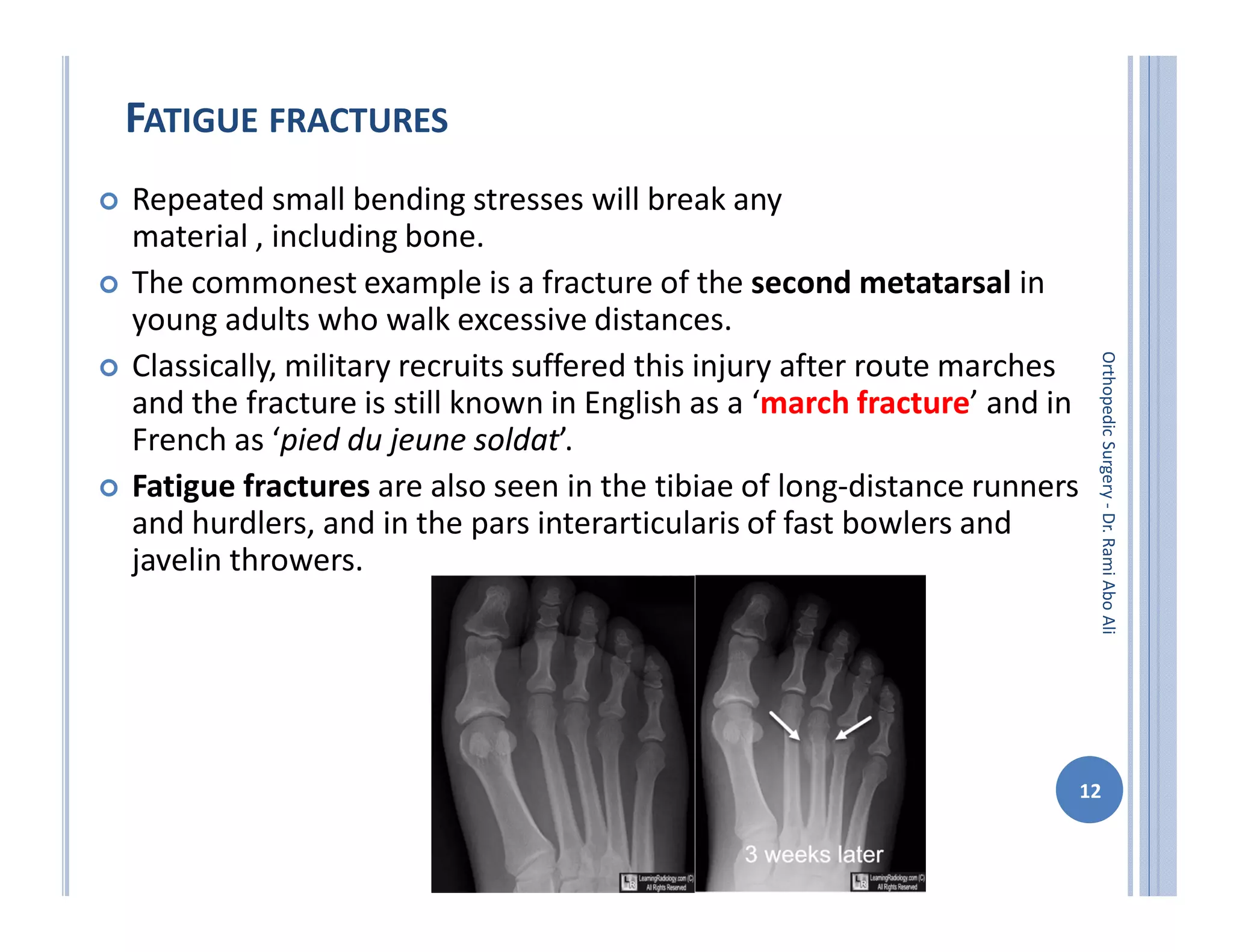
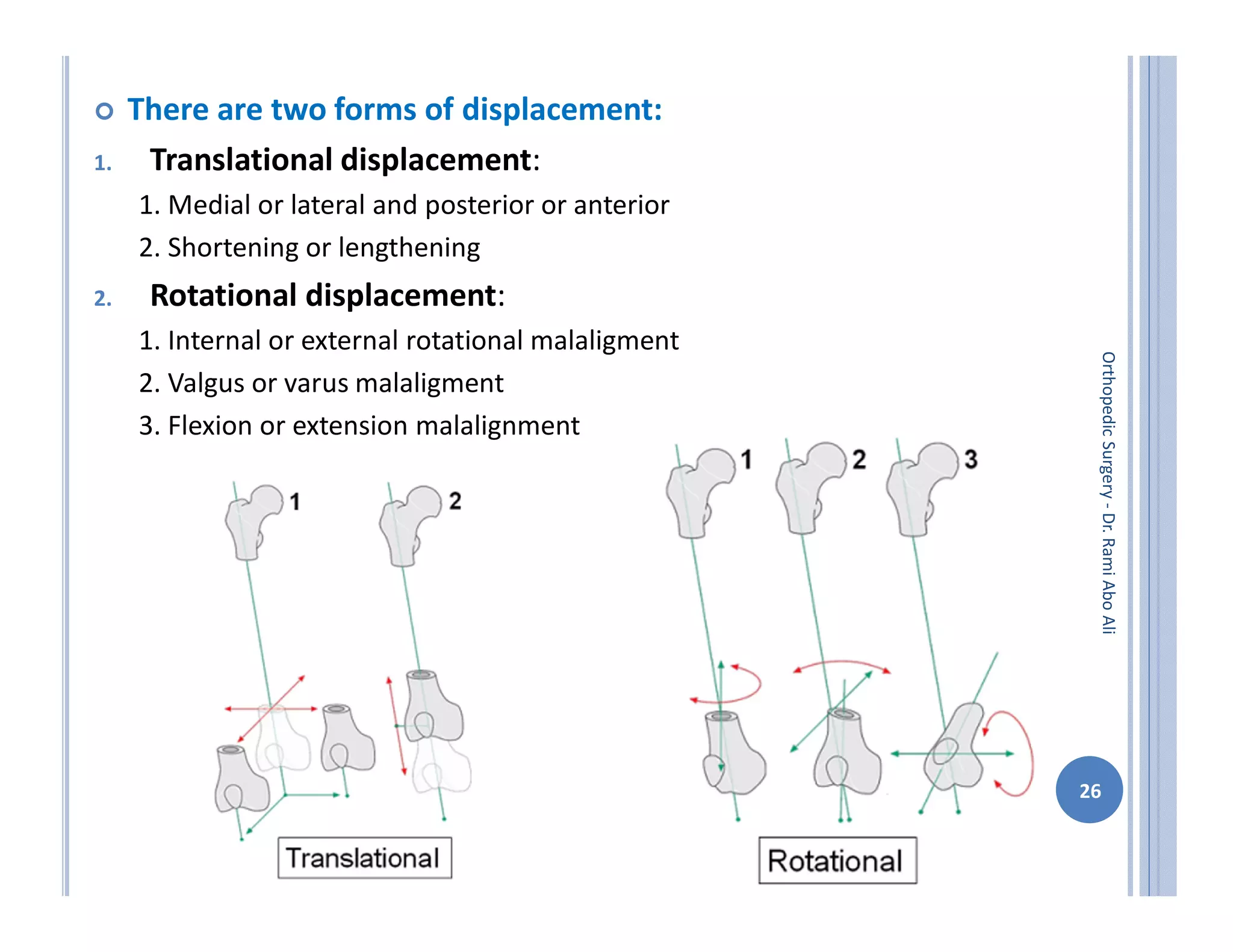
The document discusses bone formation and fracture classification. There are three types of bone formation: enchondral, where bone replaces cartilage; intramembranous, where bone develops directly from mesenchymal cells; and appositional, where new bone forms on top of existing bone. Fractures can be classified in several ways, including by shape (transverse, oblique, comminuted), location (proximal, distal), stability (stable, unstable), and degree of displacement. Fracture healing occurs either through direct union if the fracture is absolutely stable, or through callus formation involving inflammation, soft callus development, hard callus formation, and remodeling if there is movement at the fracture site.