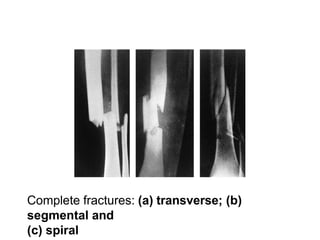
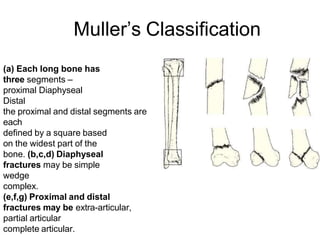
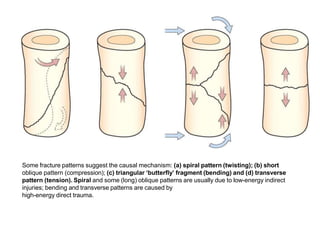
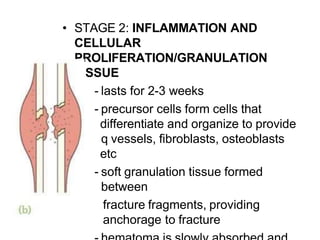
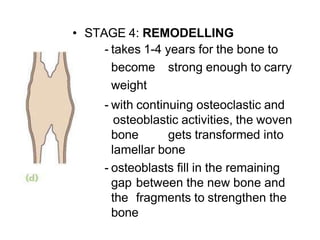
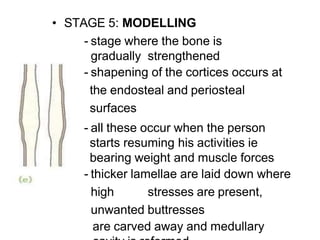
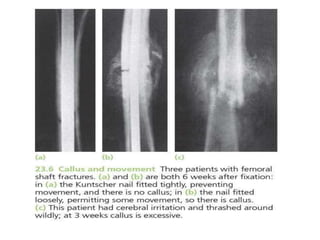
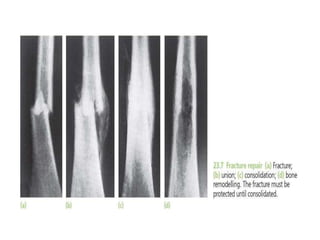
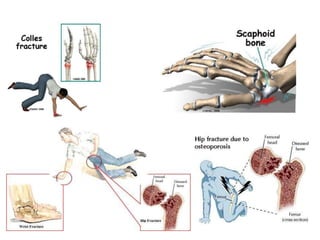
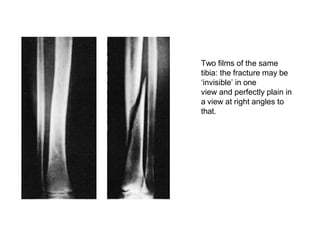
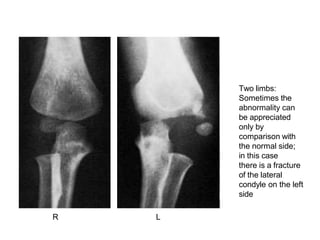
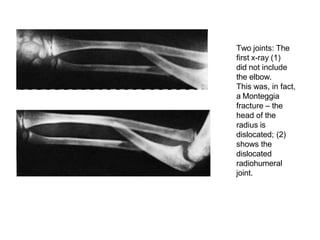
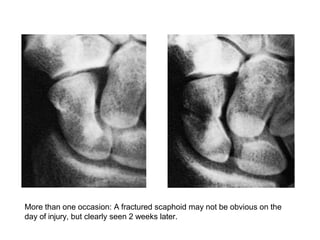
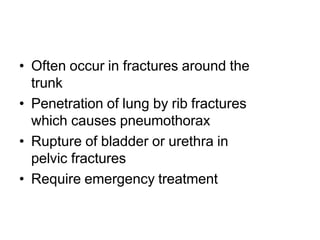
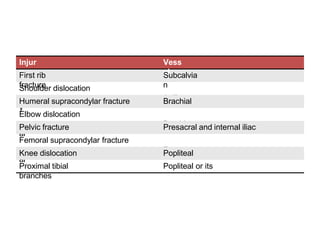
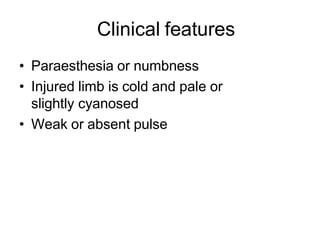
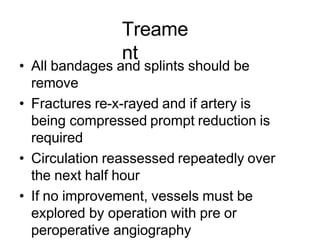
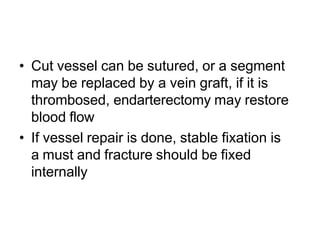
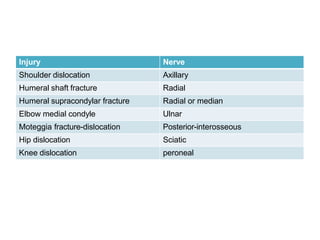
The document provides a comprehensive overview of fractures, including types, mechanisms of injury, healing stages, and clinical presentations. It outlines the classification of fractures, mechanisms of displacement, diagnostic imaging requirements, and potential complications associated with fractures. In addition, it discusses the management protocols for different types of injuries and emphasizes the importance of thorough examination and history-taking for accurate diagnosis and treatment.