This document discusses peripheral neuropathy and provides details on various types including:
- Peripheral neuropathy can affect nerves in the arms, legs, or other areas and be classified by pathology, size of nerves affected, or function (sensory, motor, autonomic).
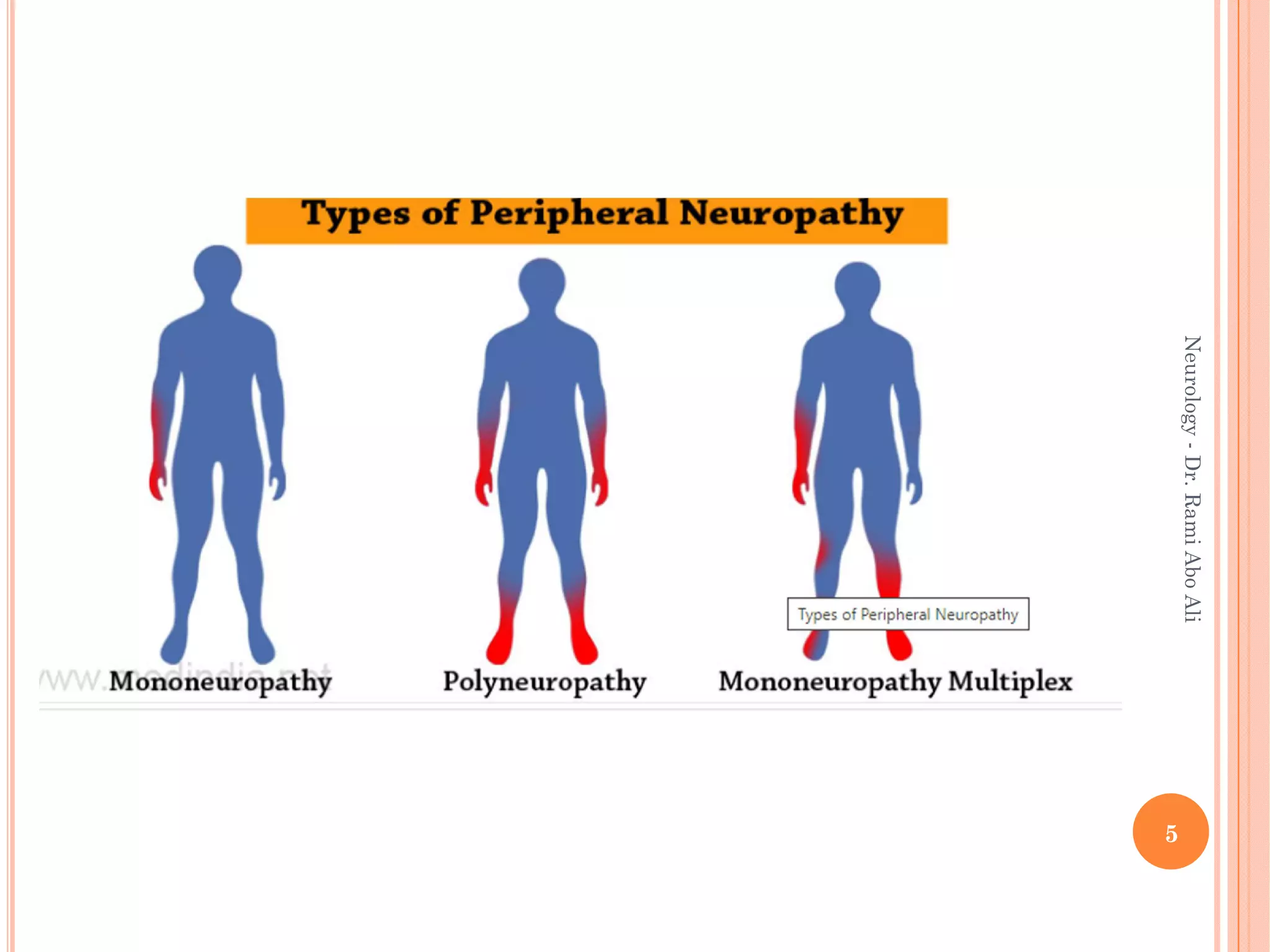
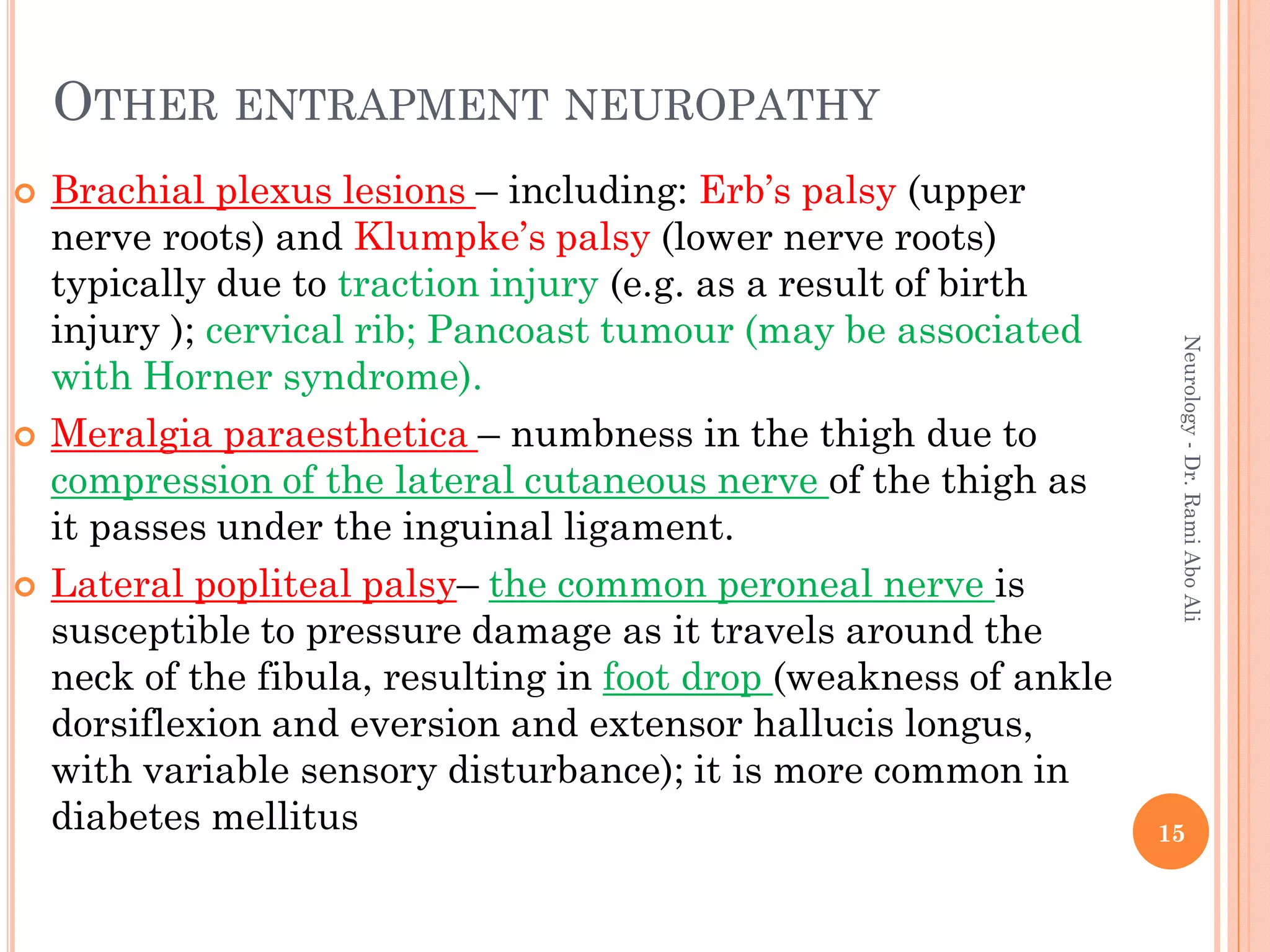
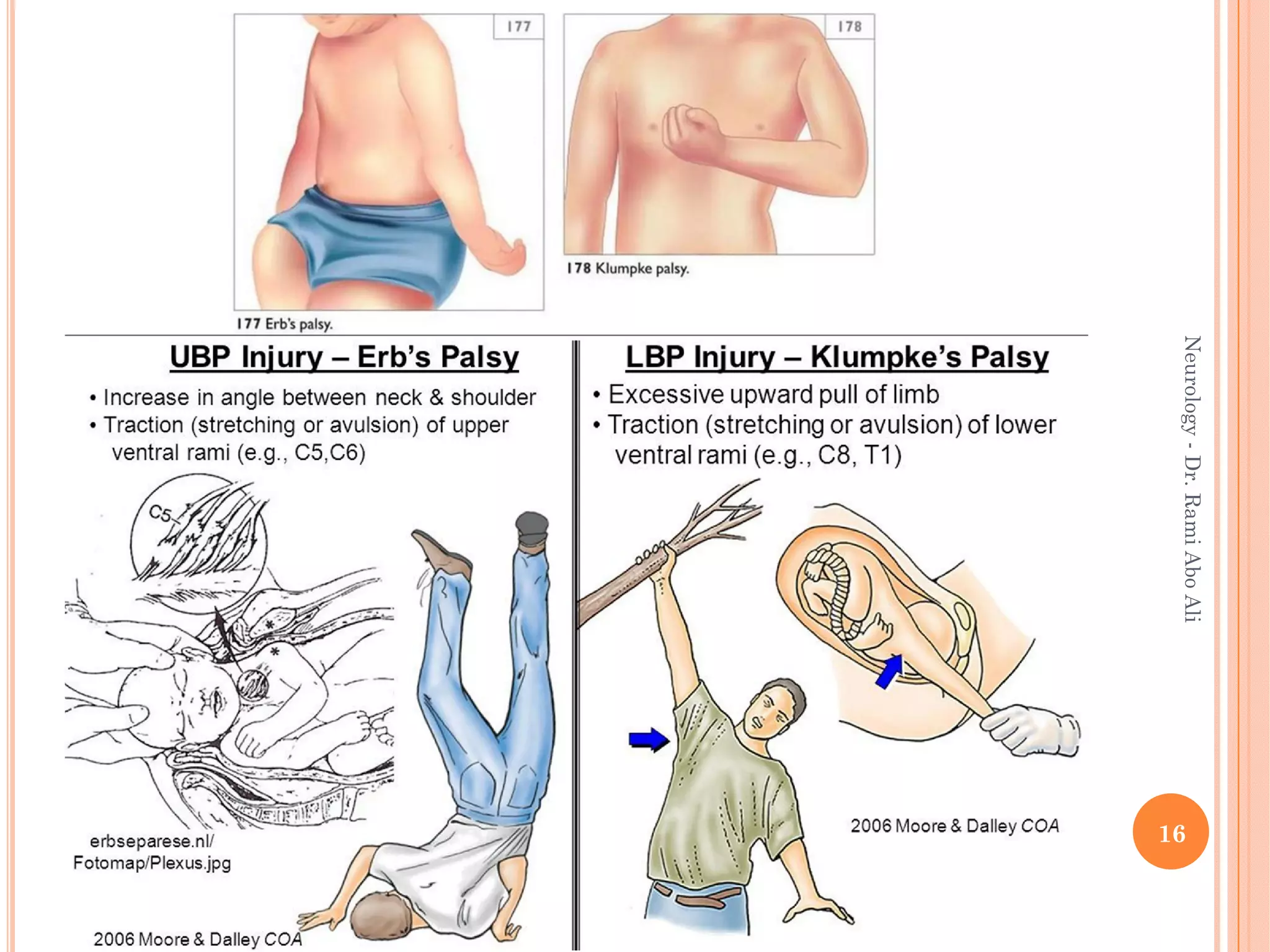
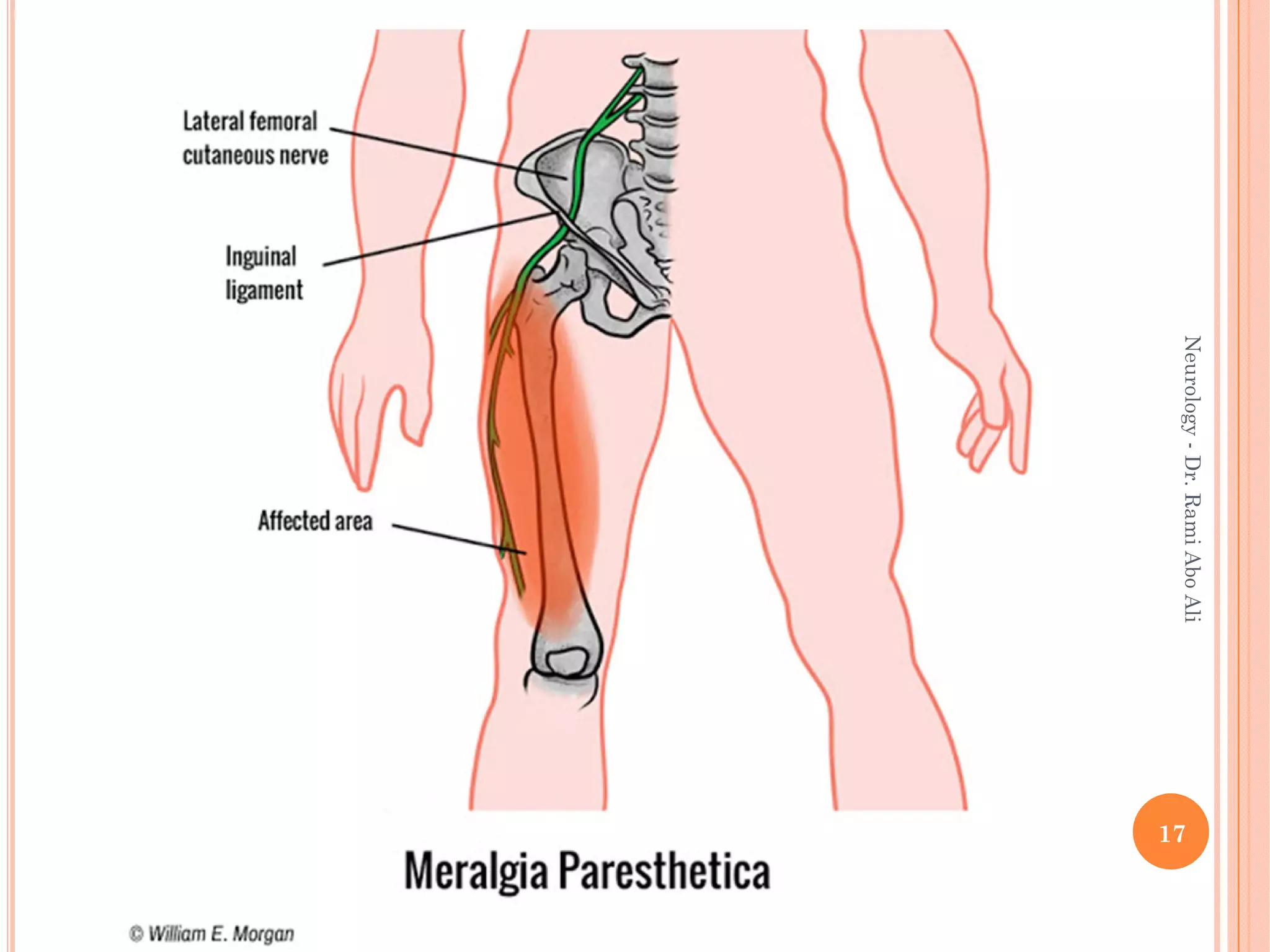
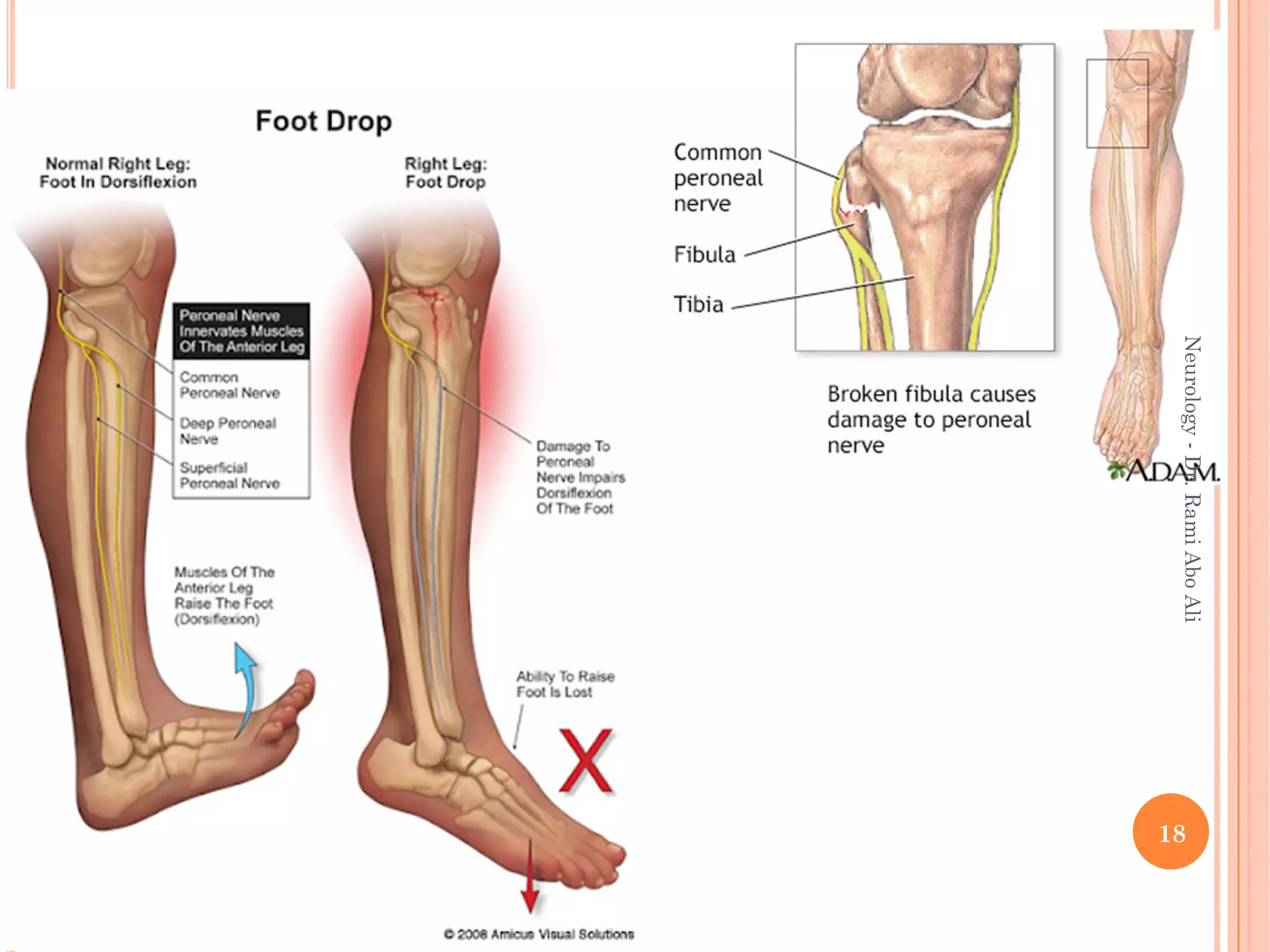
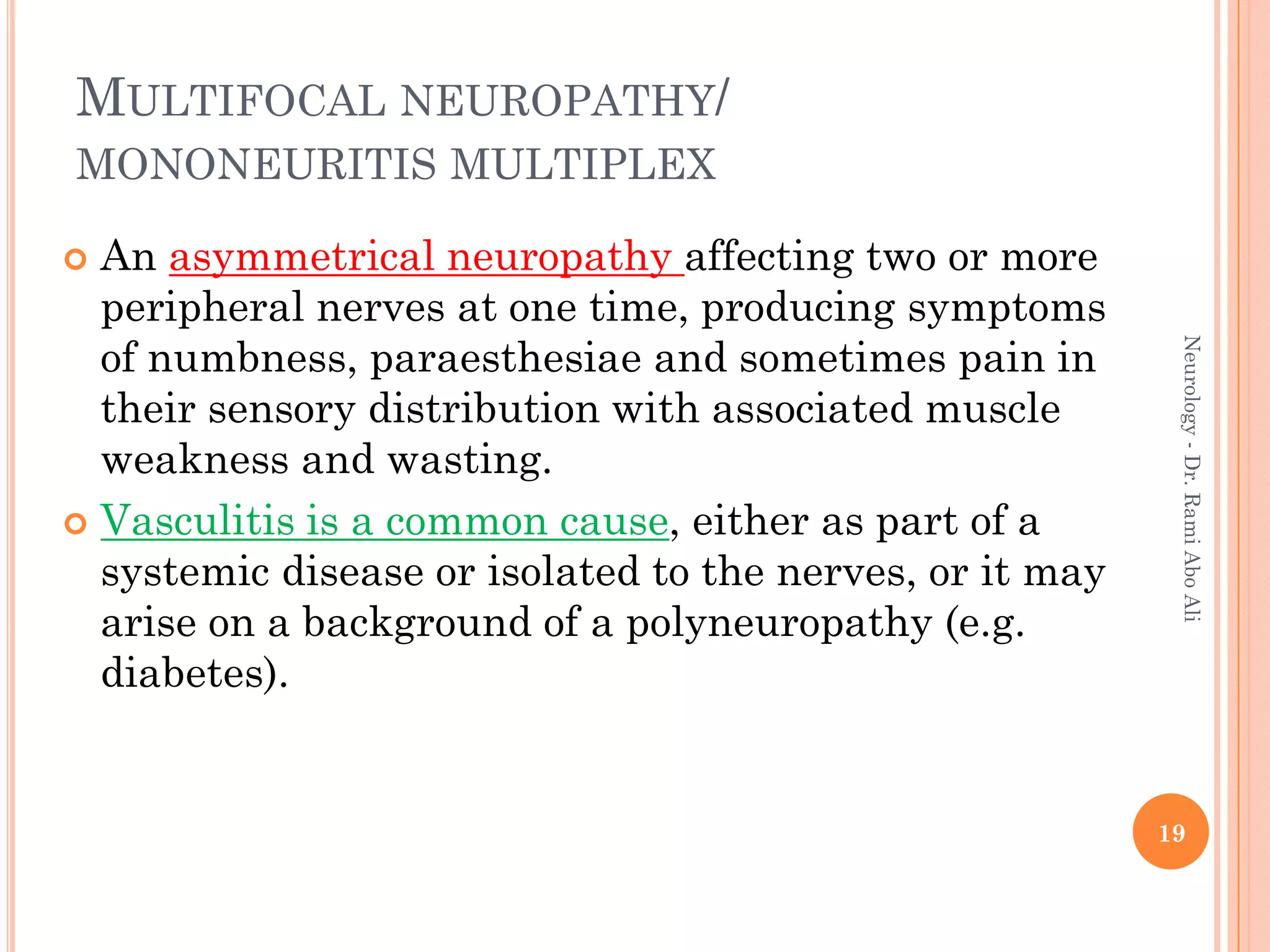
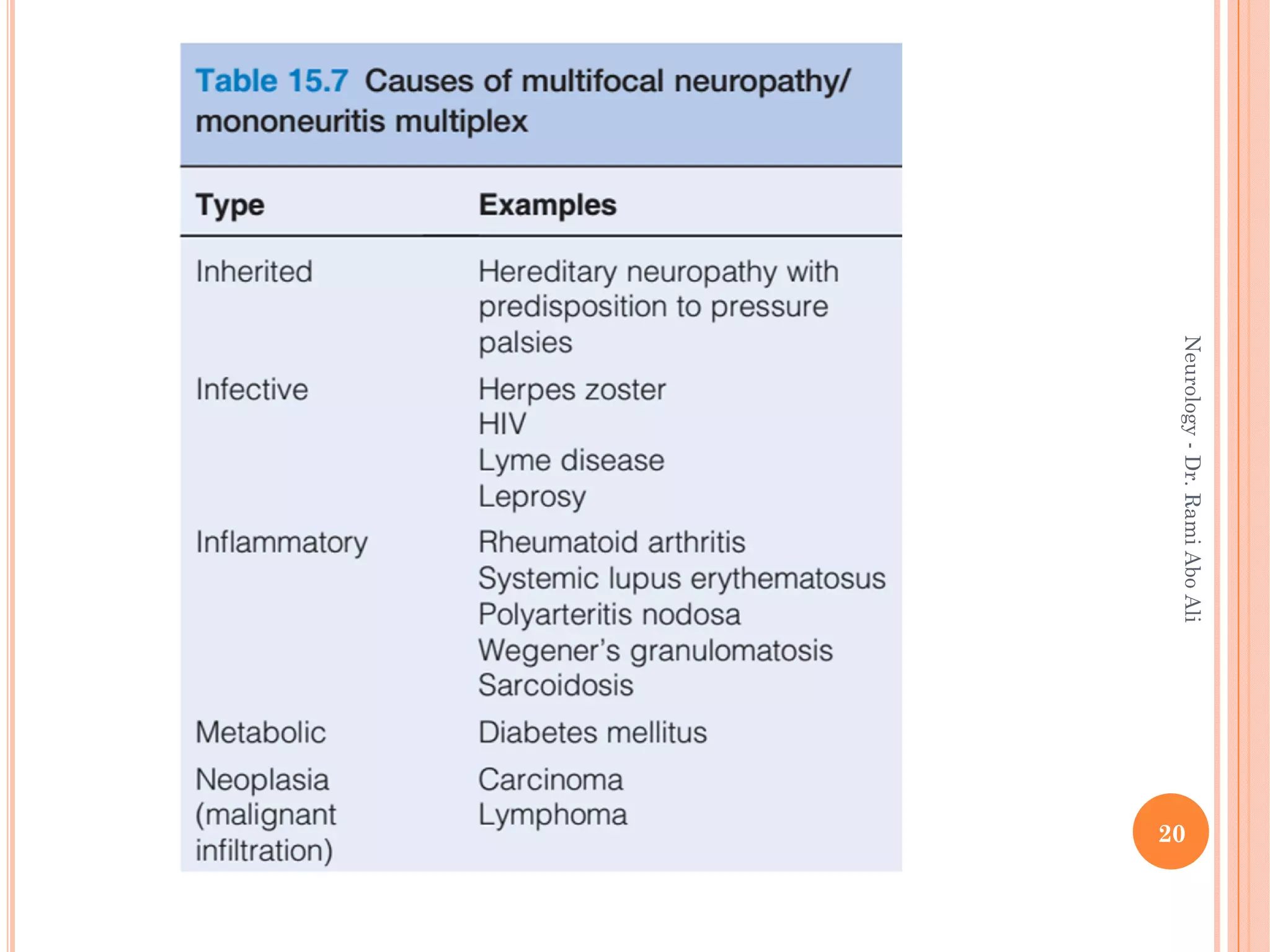
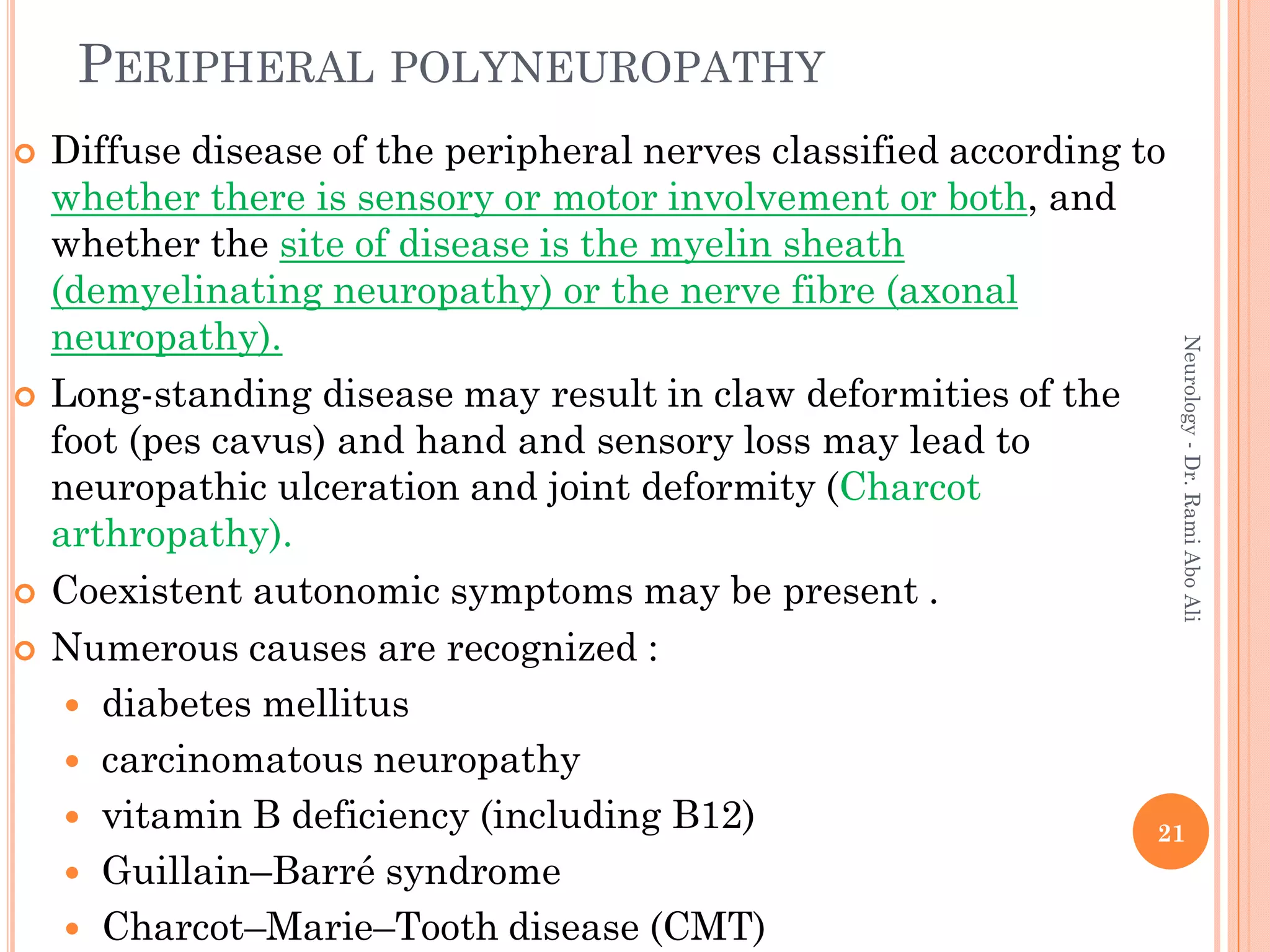
- Specific types discussed include mononeuropathies which affect individual nerves, polyneuropathies which affect multiple nerves symmetrically, and plexopathies.
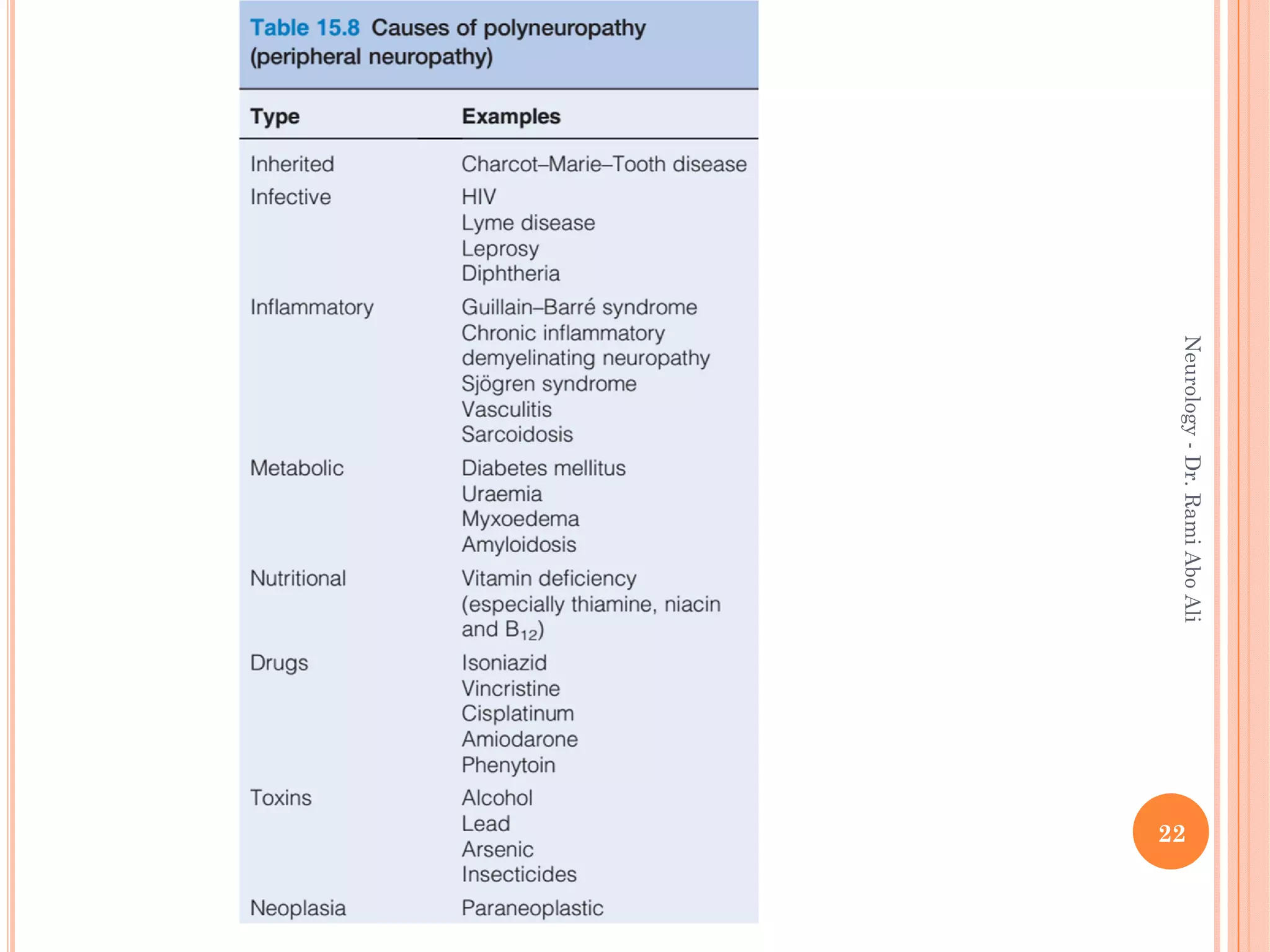
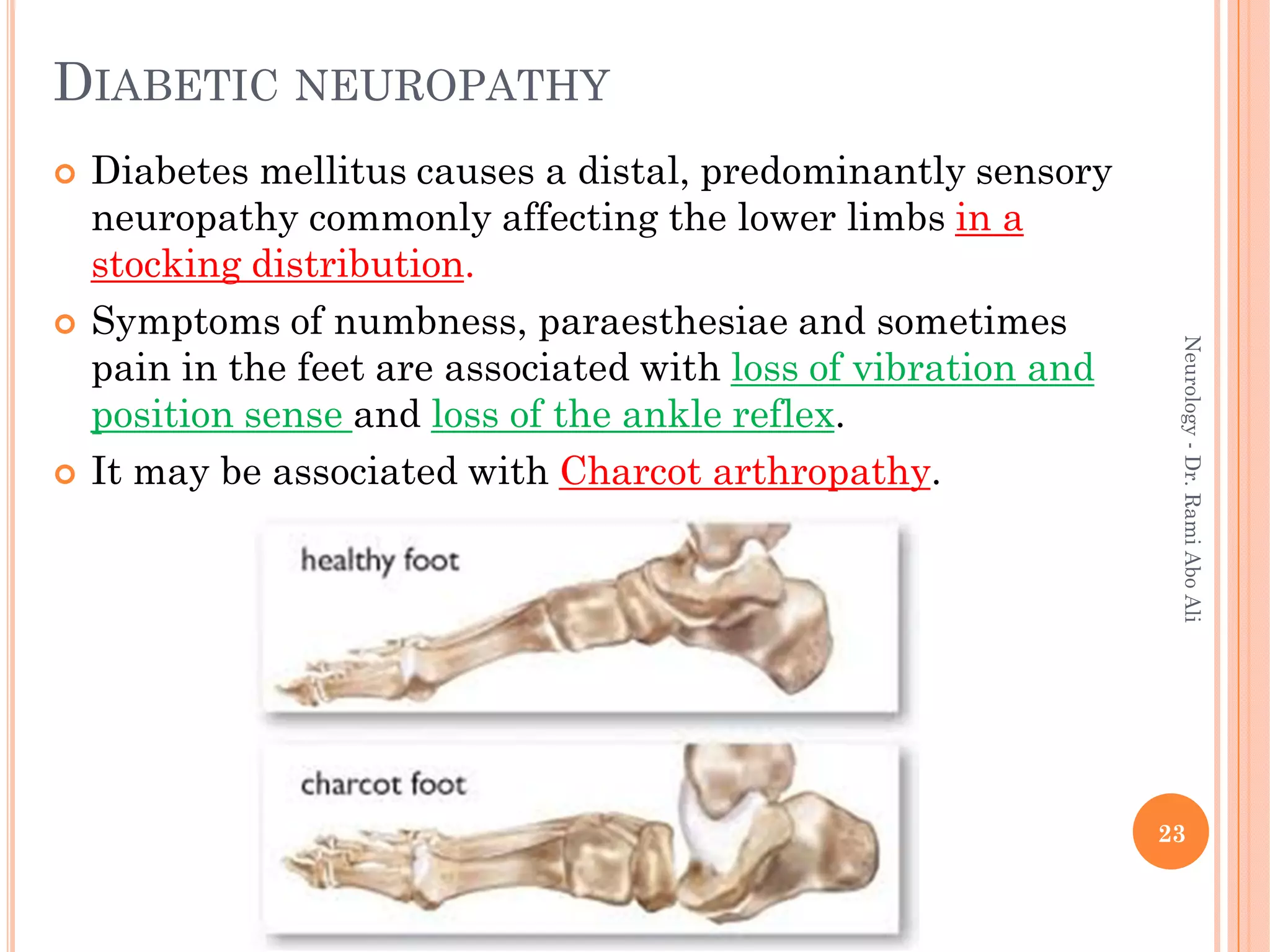
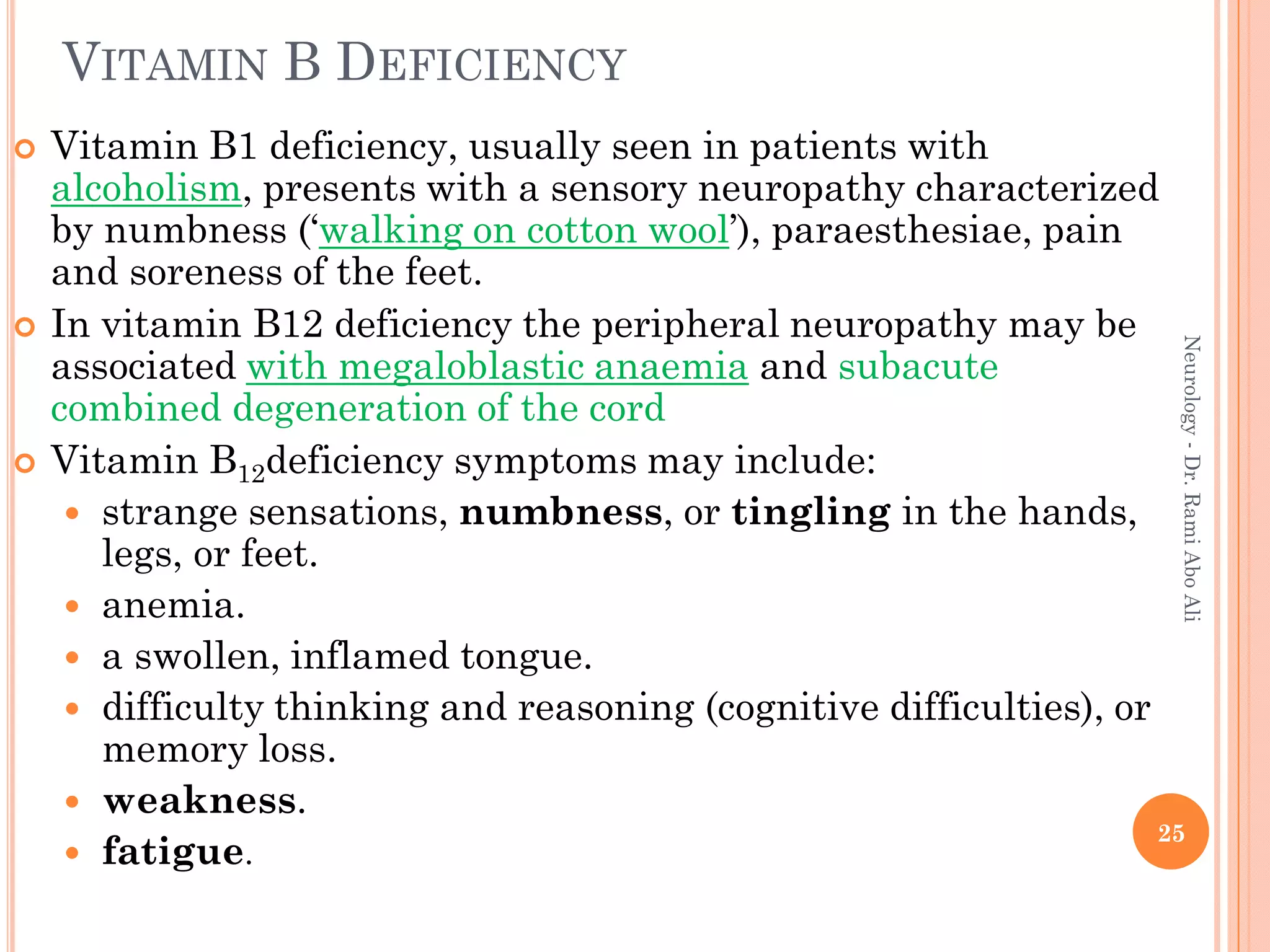
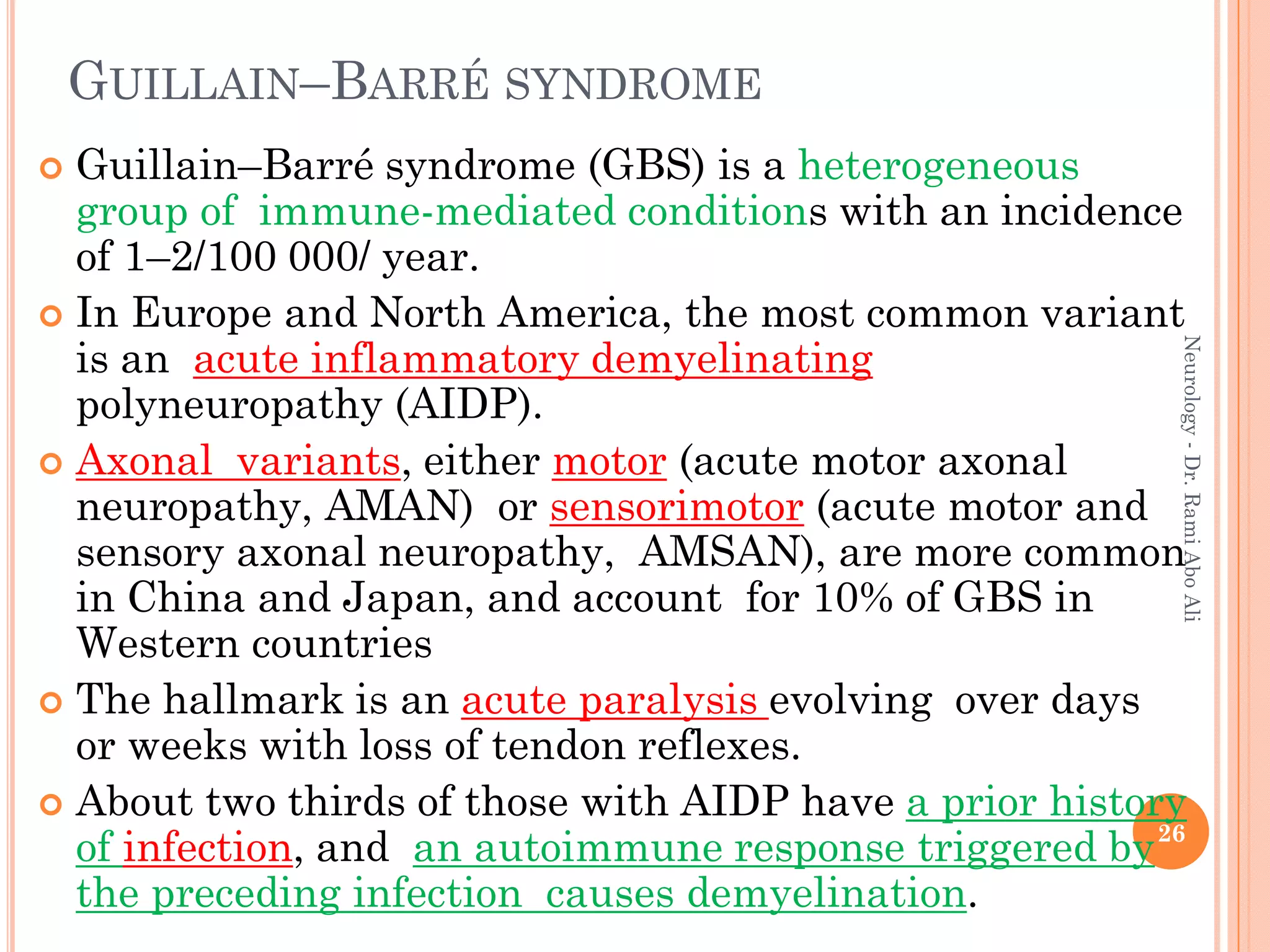
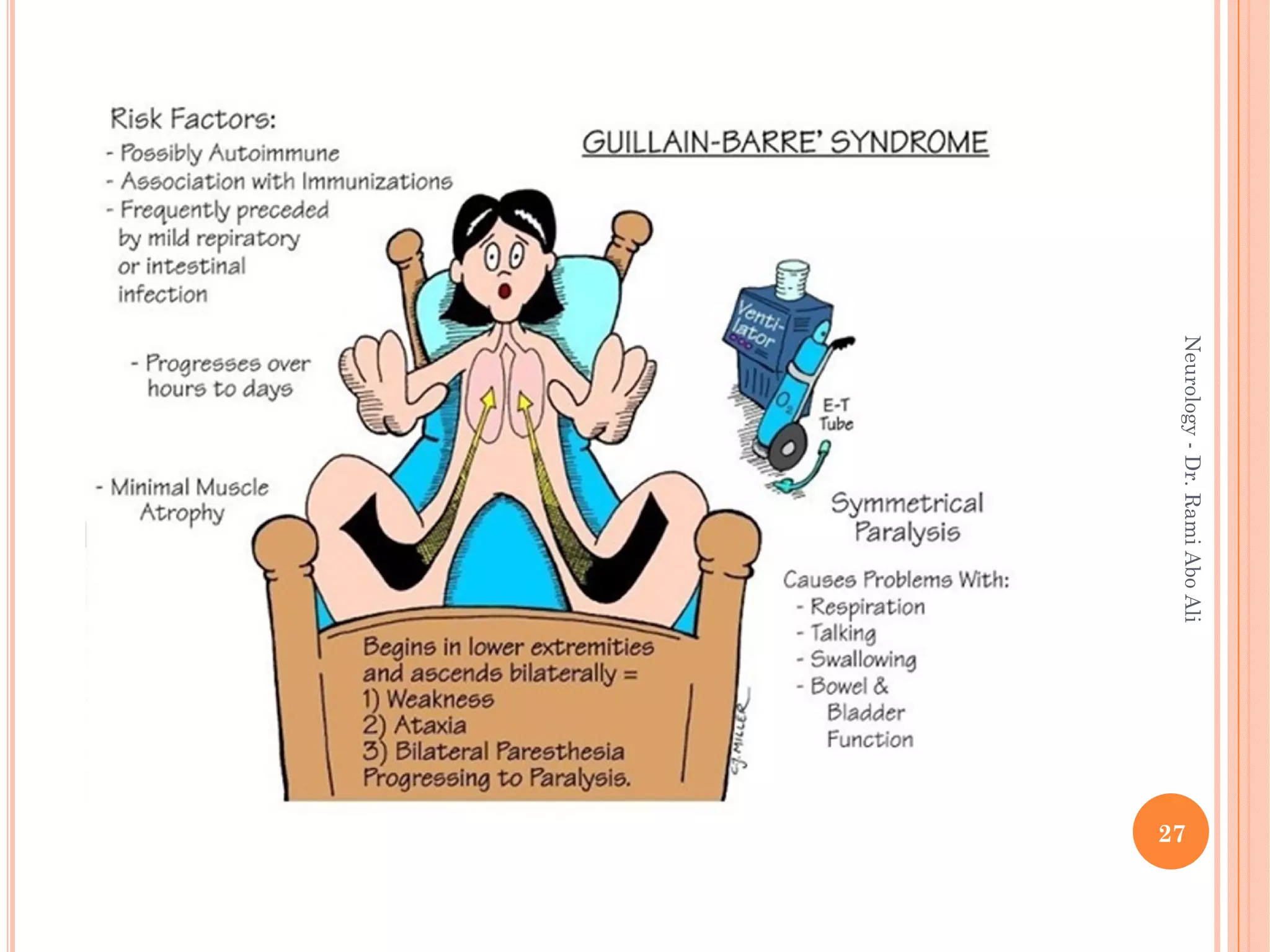
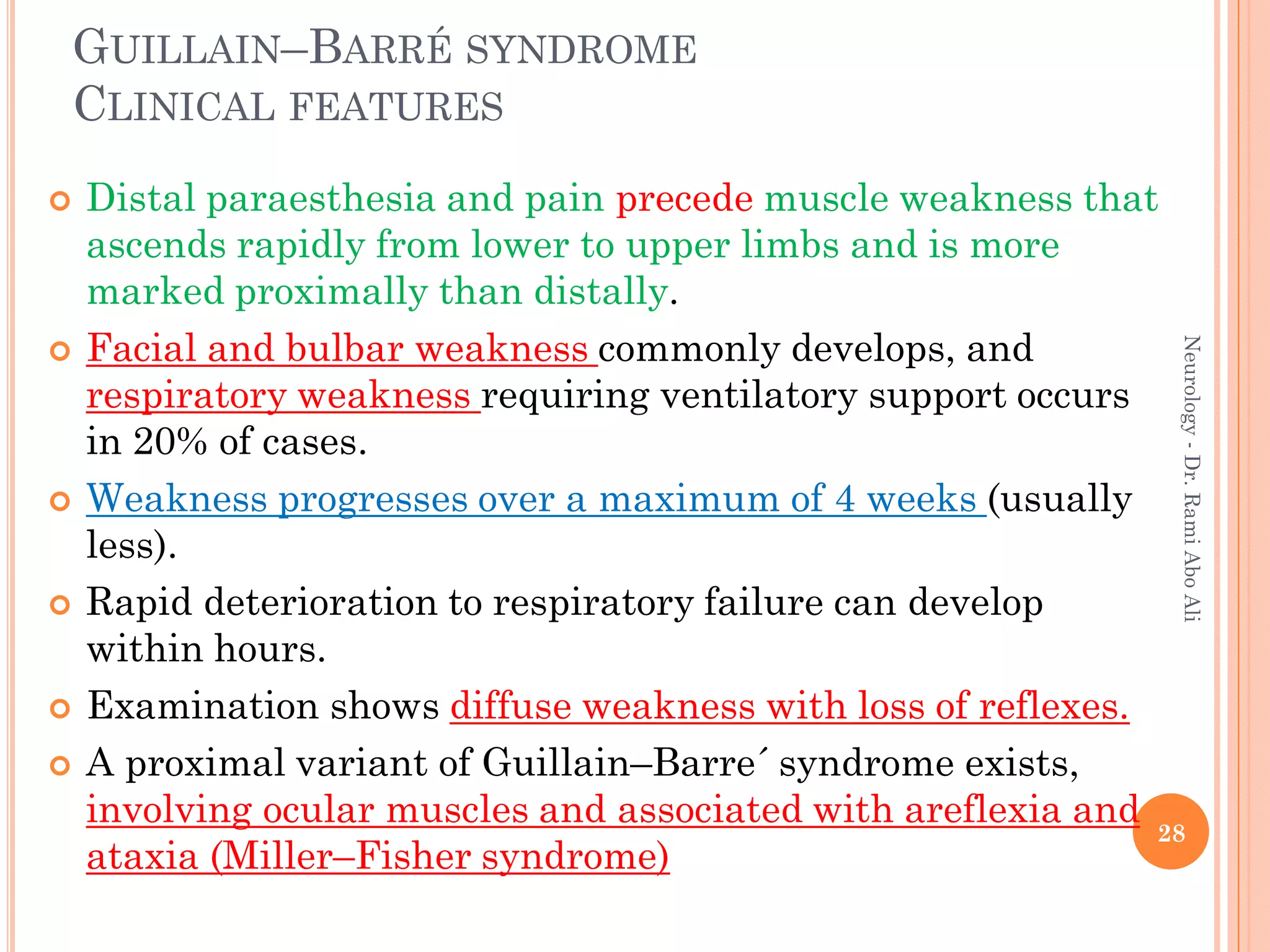
- Causes include metabolic, infectious, inflammatory, toxic, and hereditary factors. Specific conditions like diabetes, Guillain-Barré syndrome, and Charcot-Marie-Tooth disease are examined in depth.
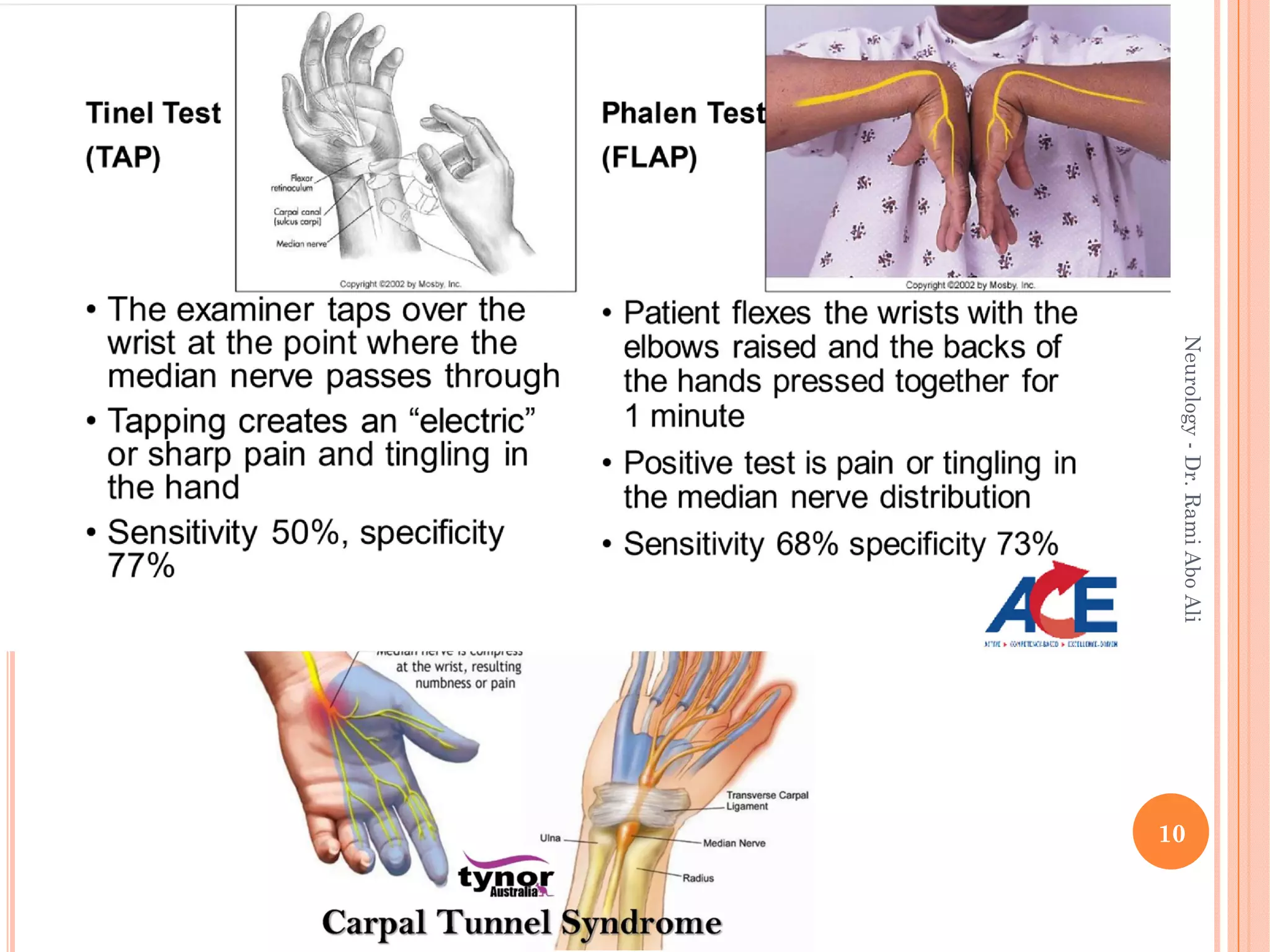
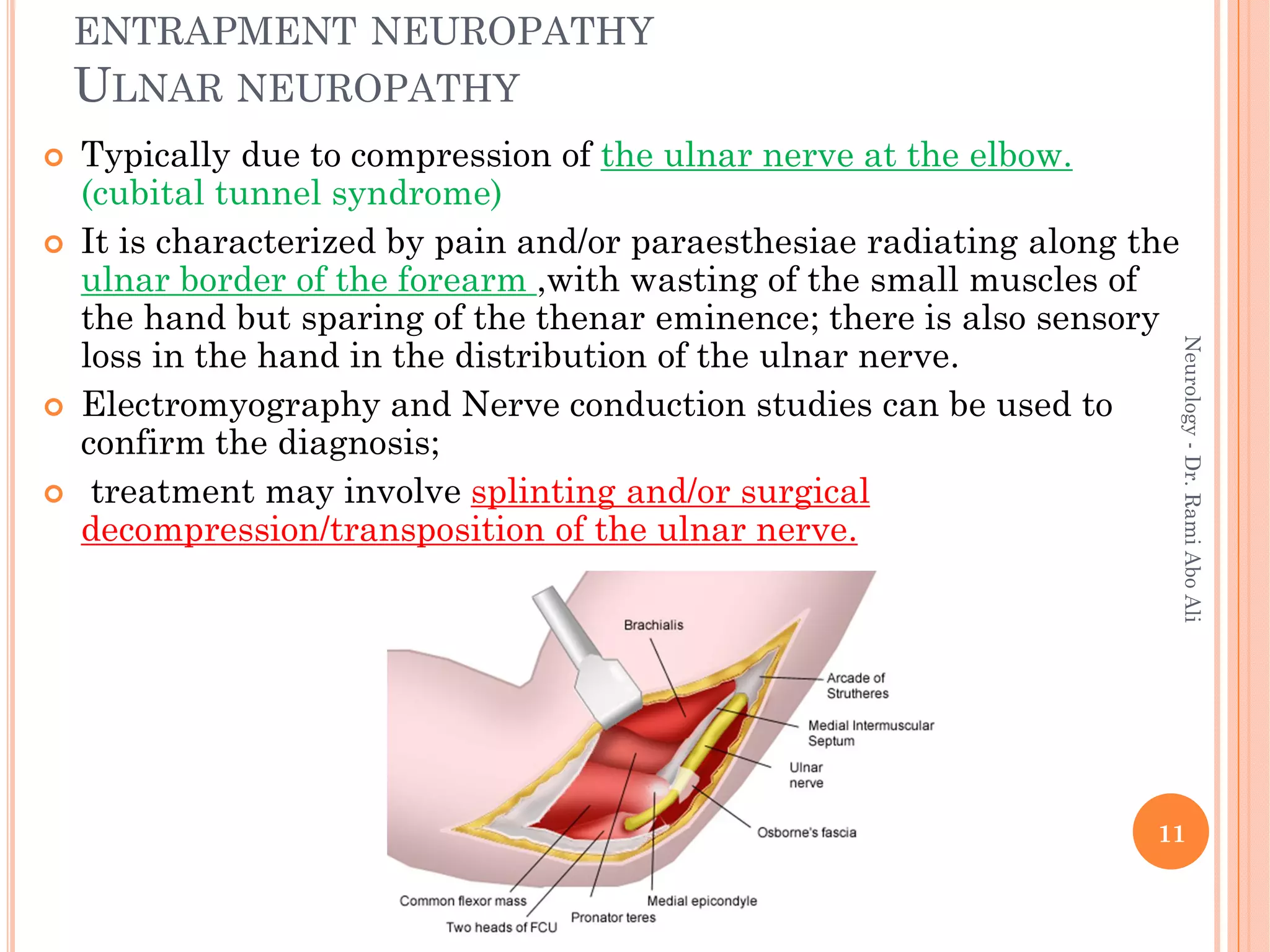
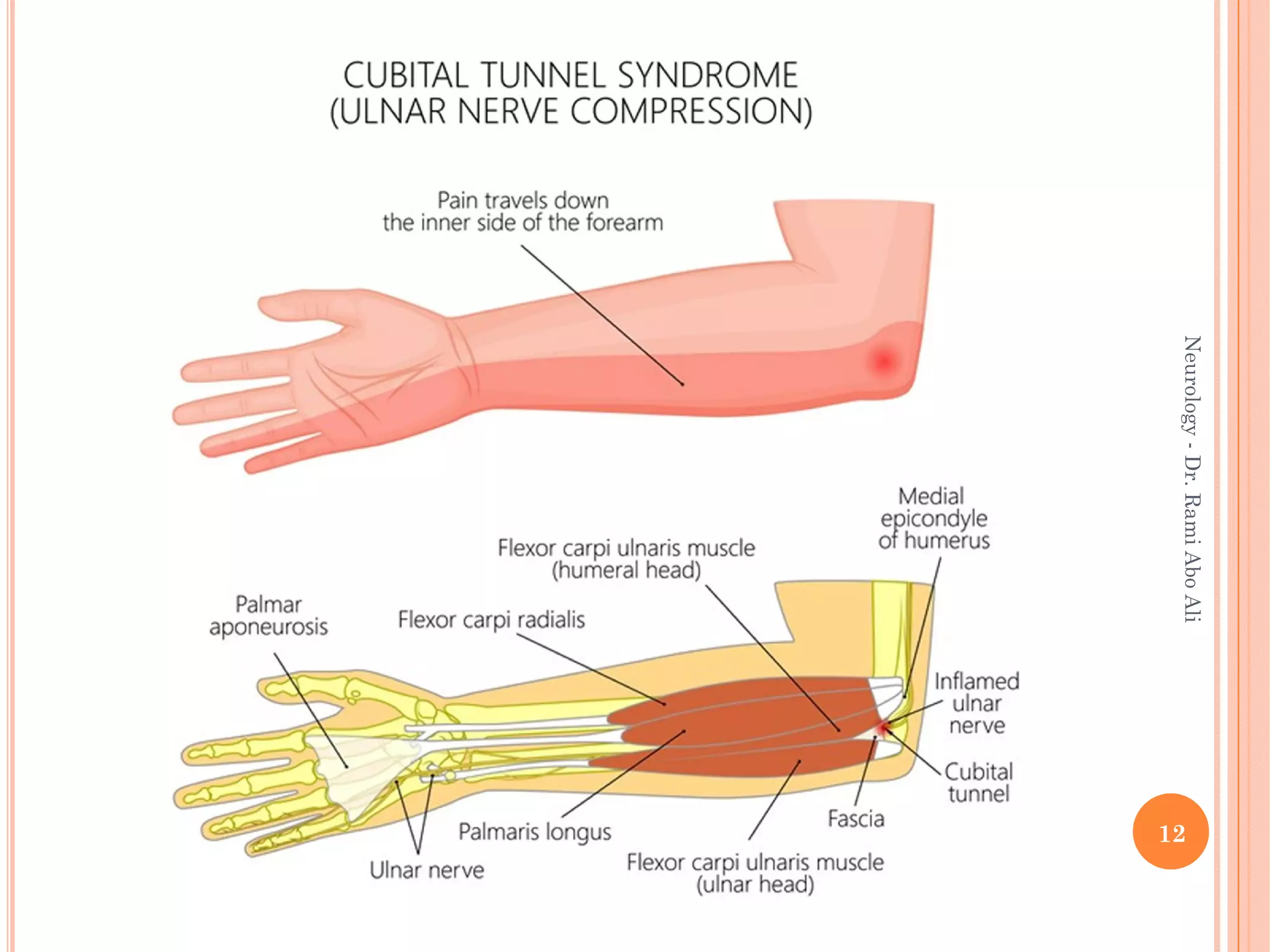
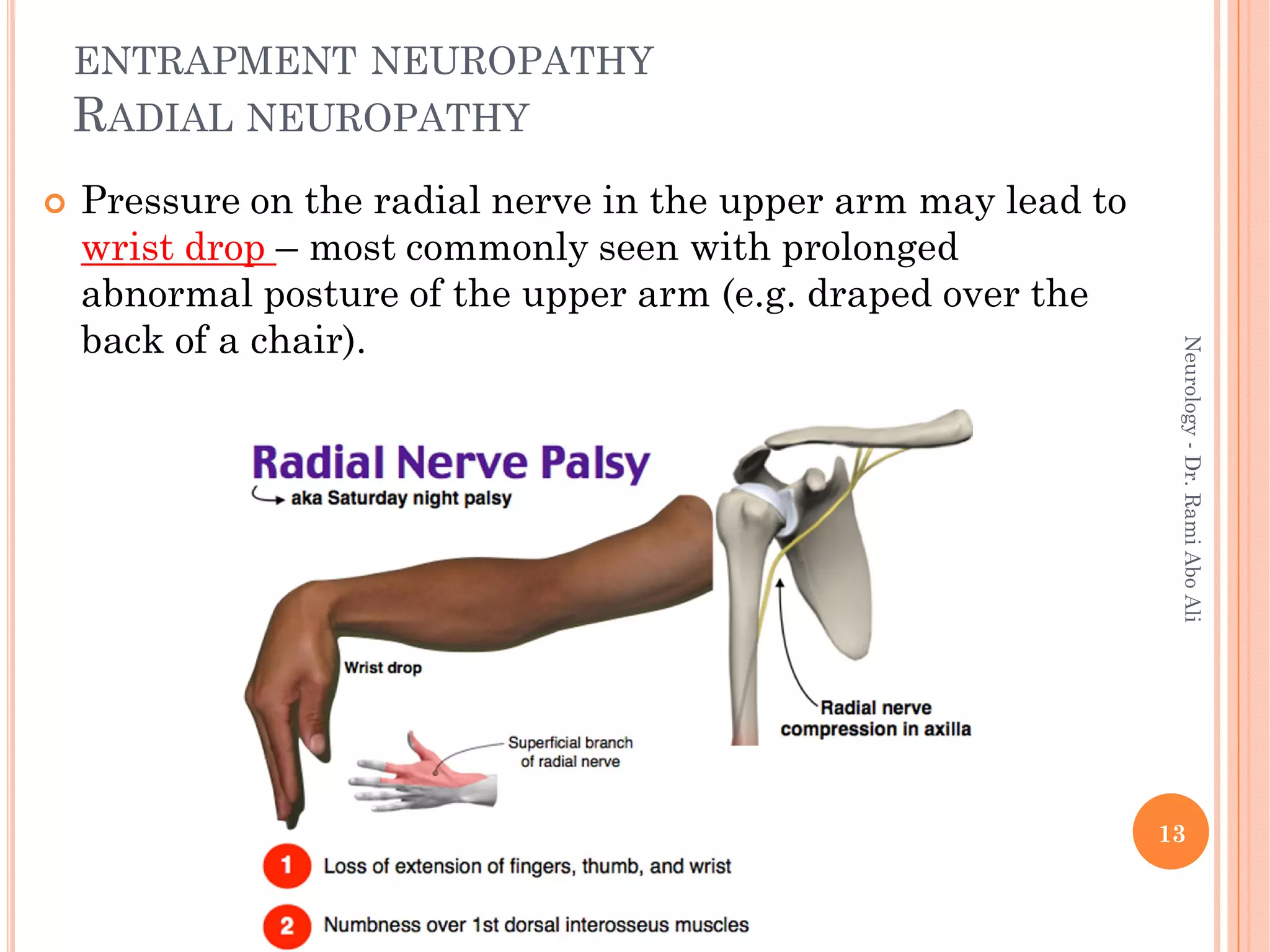
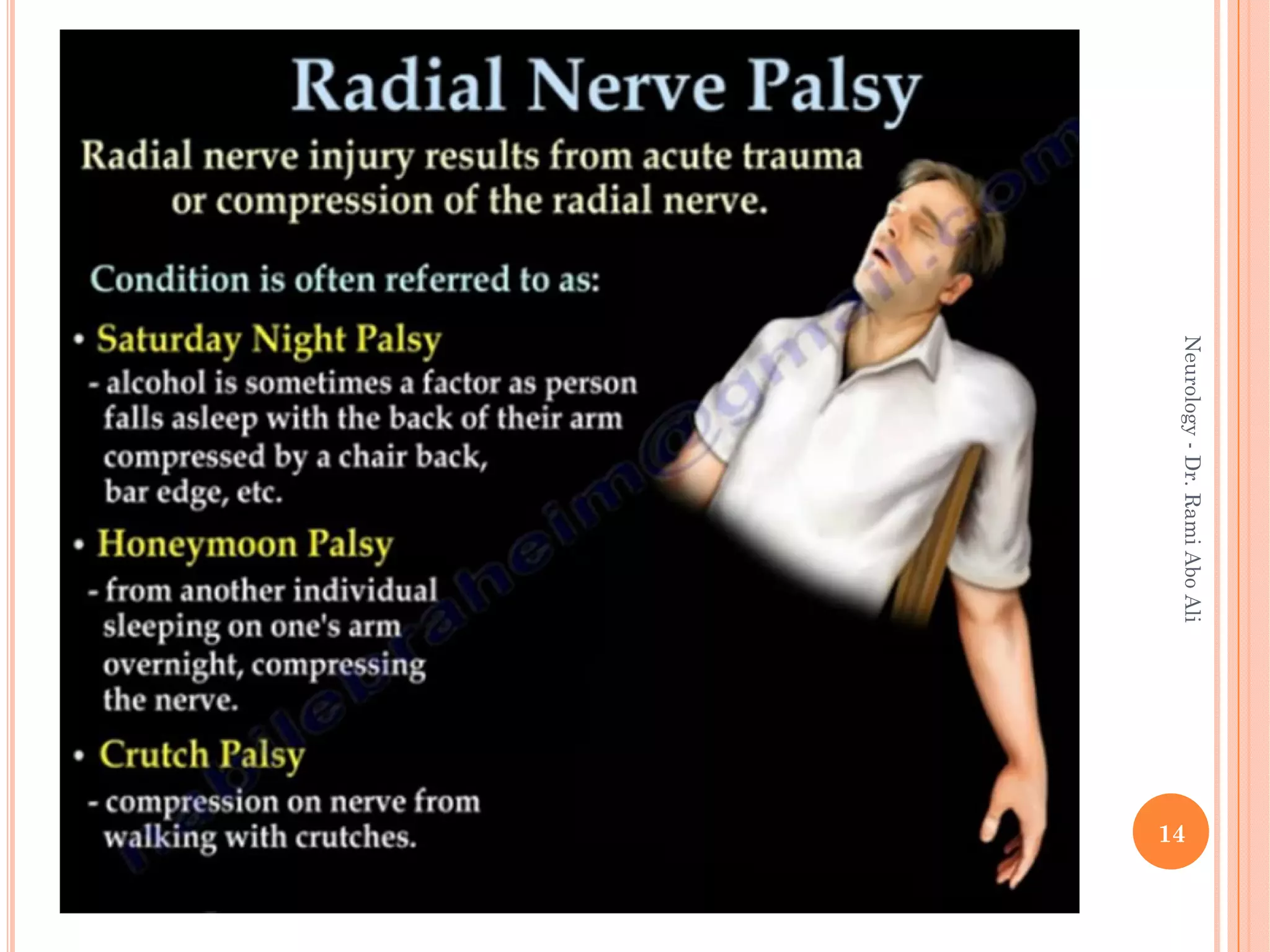
- Entrapment neuropathies at sites like the carpal