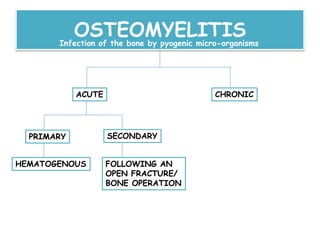
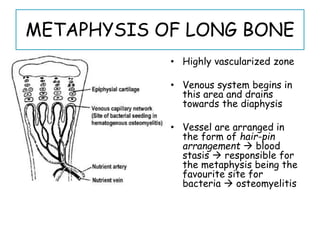
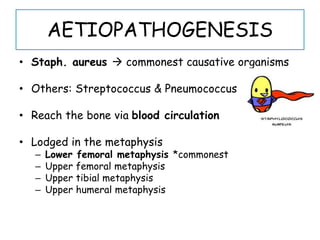
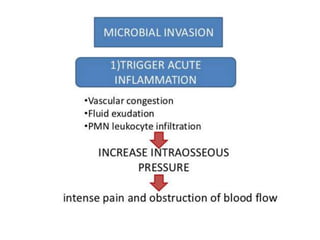
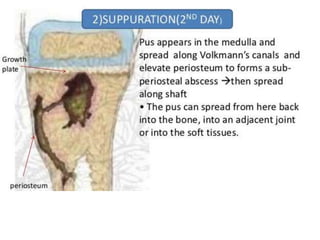
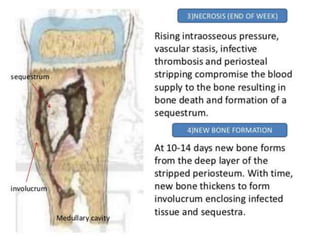
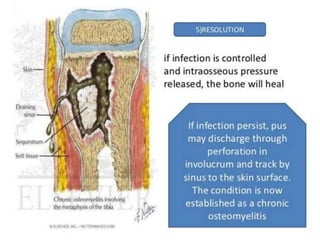
Acute osteomyelitis is a bone infection commonly caused by Staphylococcus aureus, primarily affecting the metaphysis of long bones, particularly in children. Diagnosis is based on clinical symptoms and supportive investigations, while treatment involves early antibiotic administration and potentially surgical intervention for abscess drainage if symptoms persist beyond 48 hours. Complications may include chronic osteomyelitis and septic complications, with prevention focusing on proper management of open fractures.