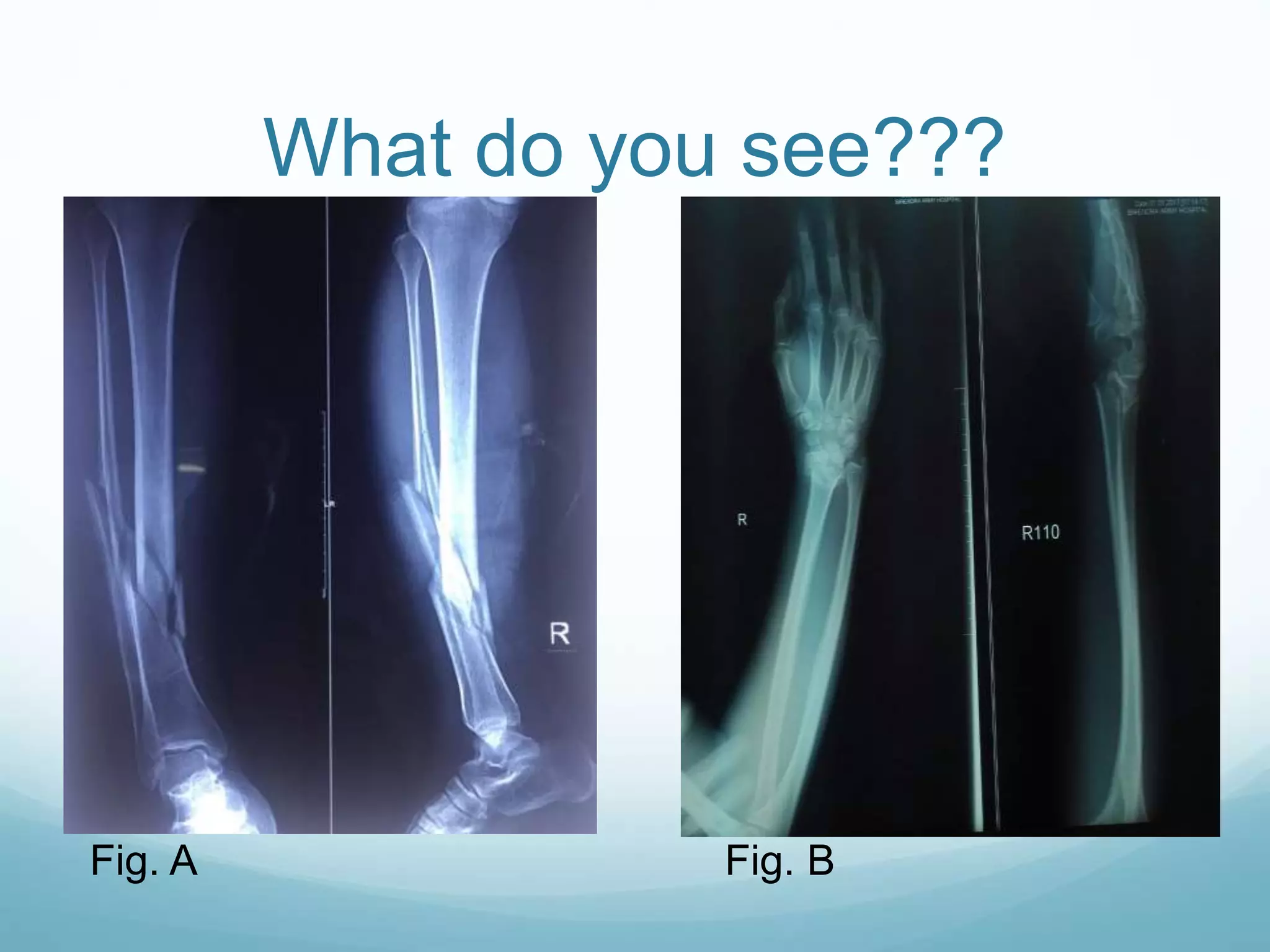
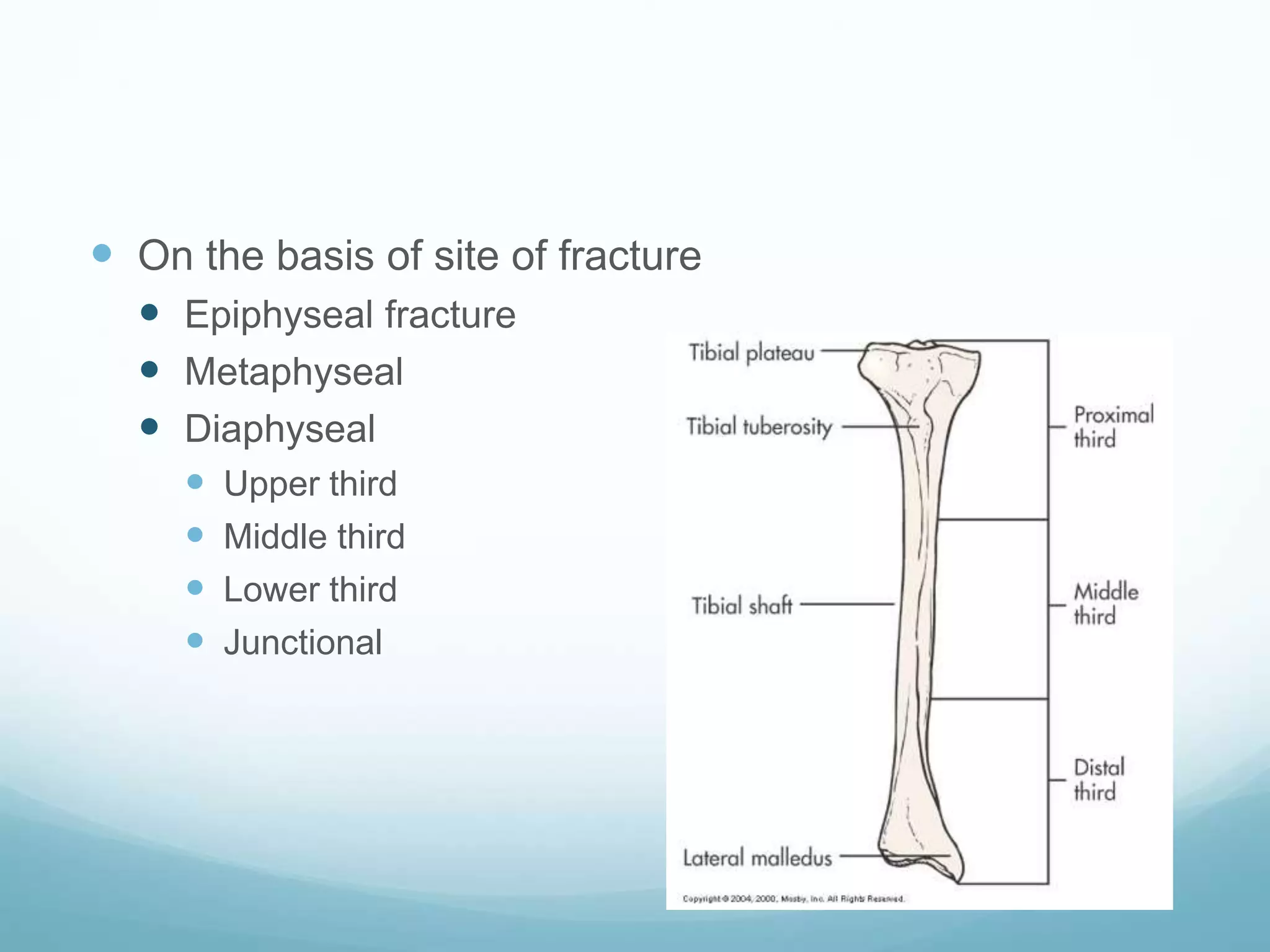
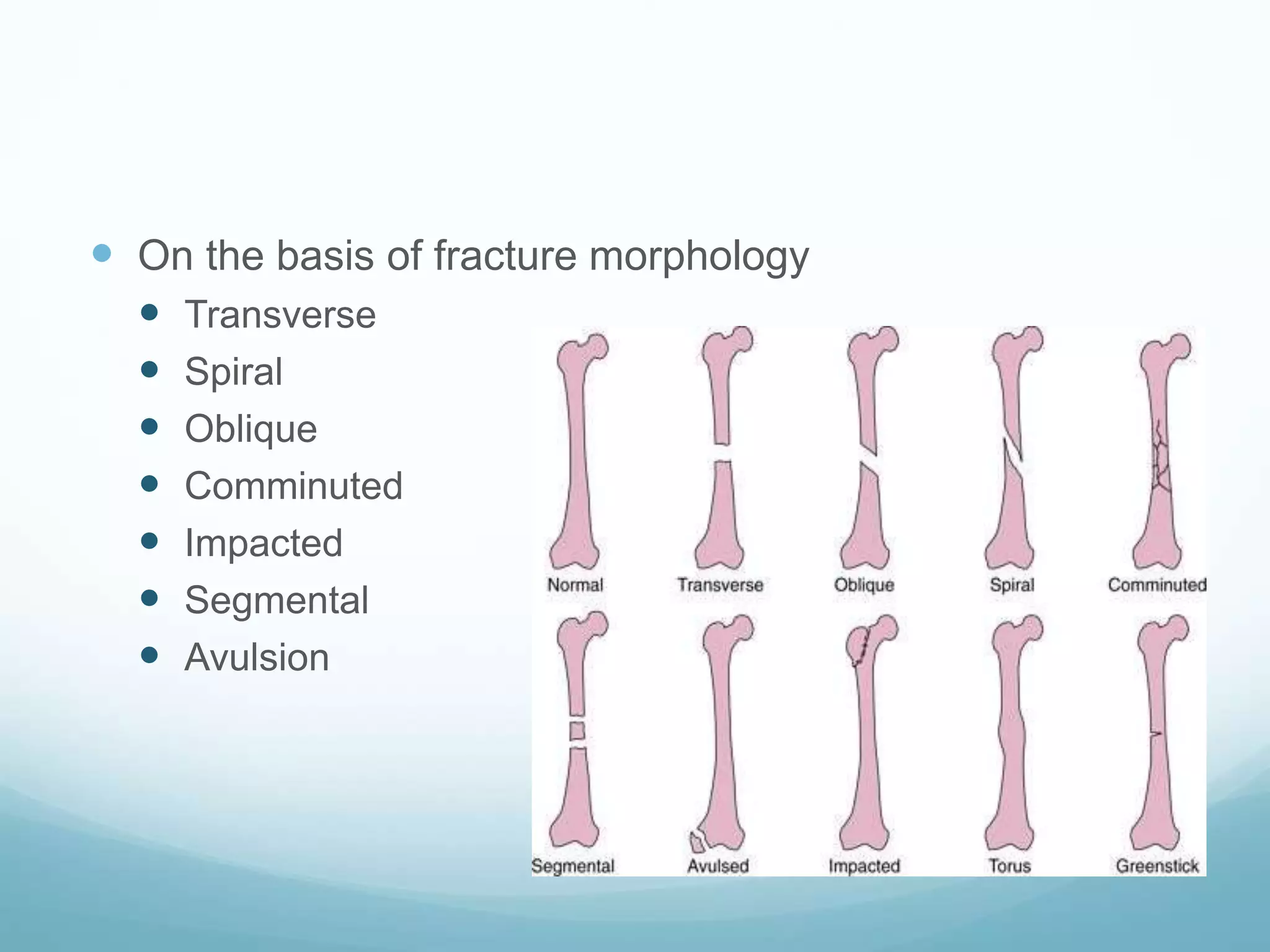
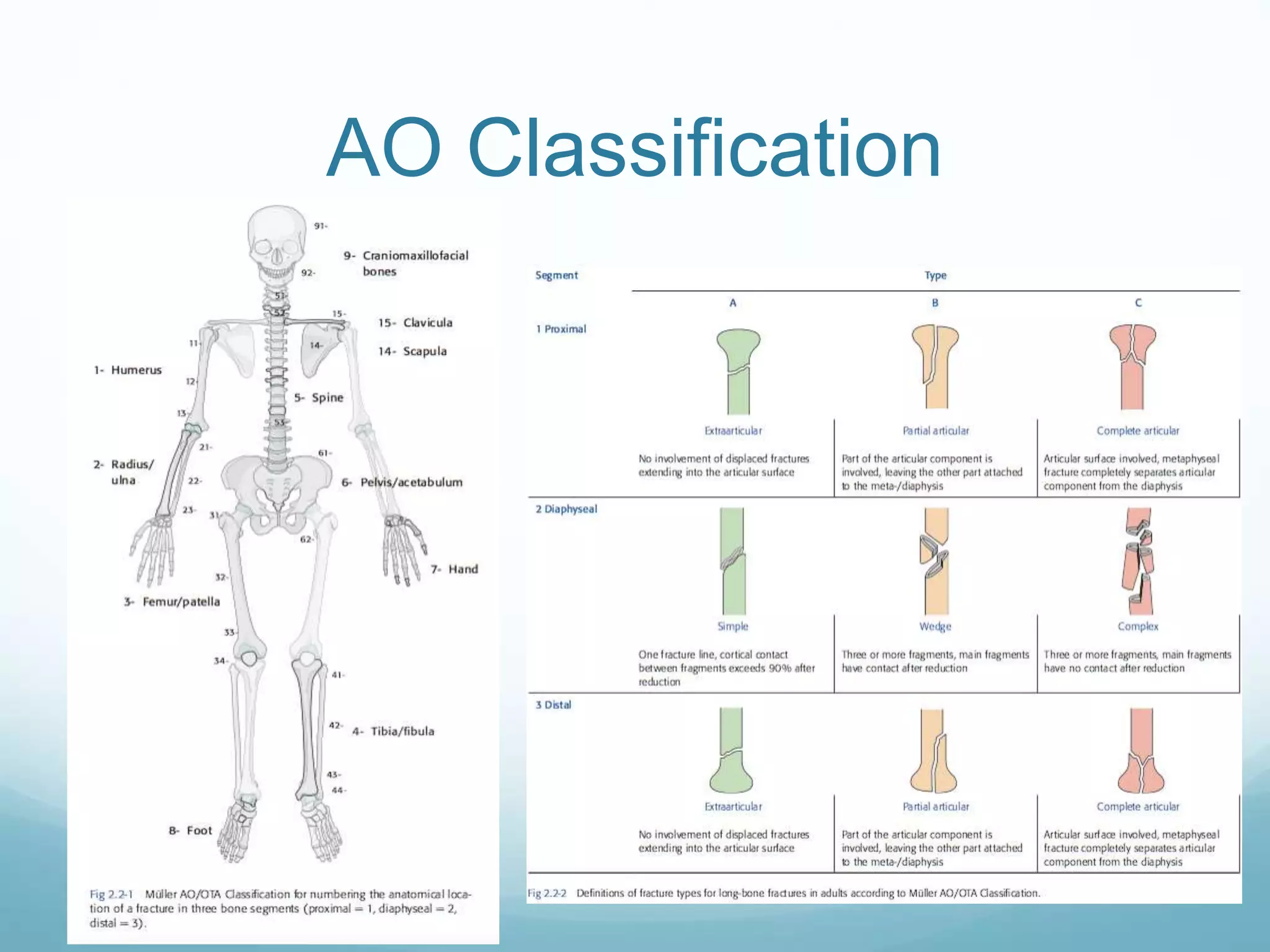
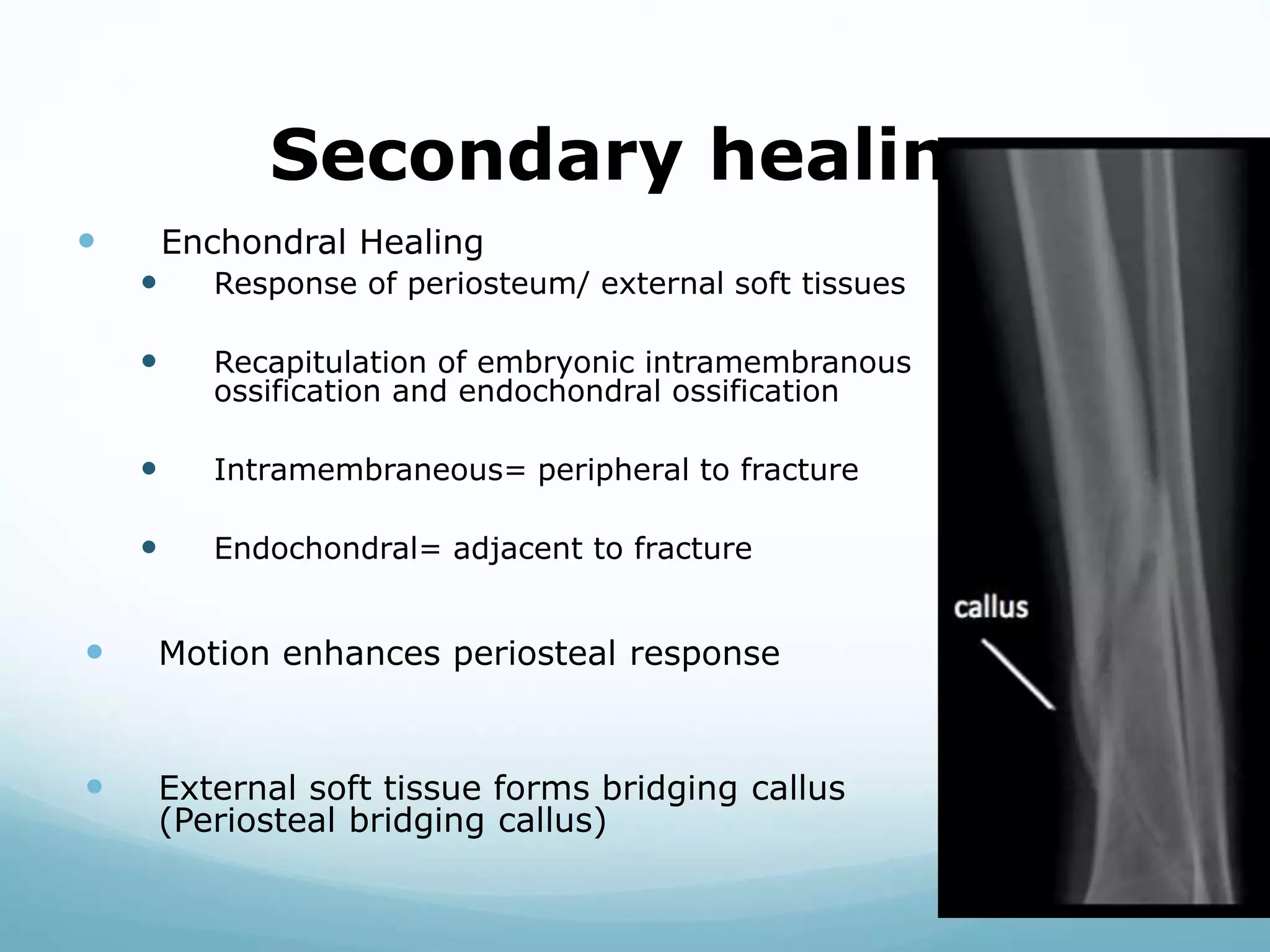
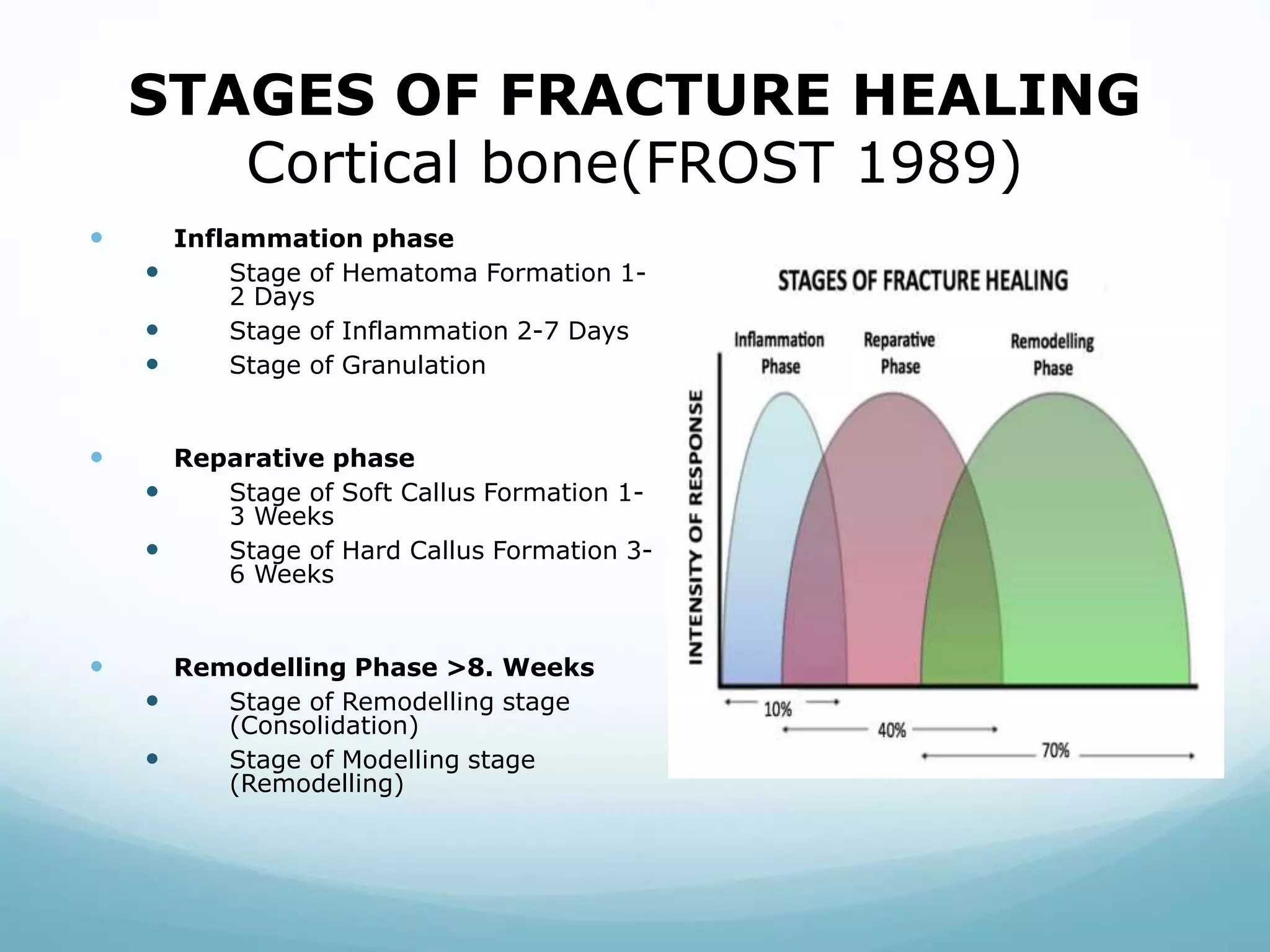
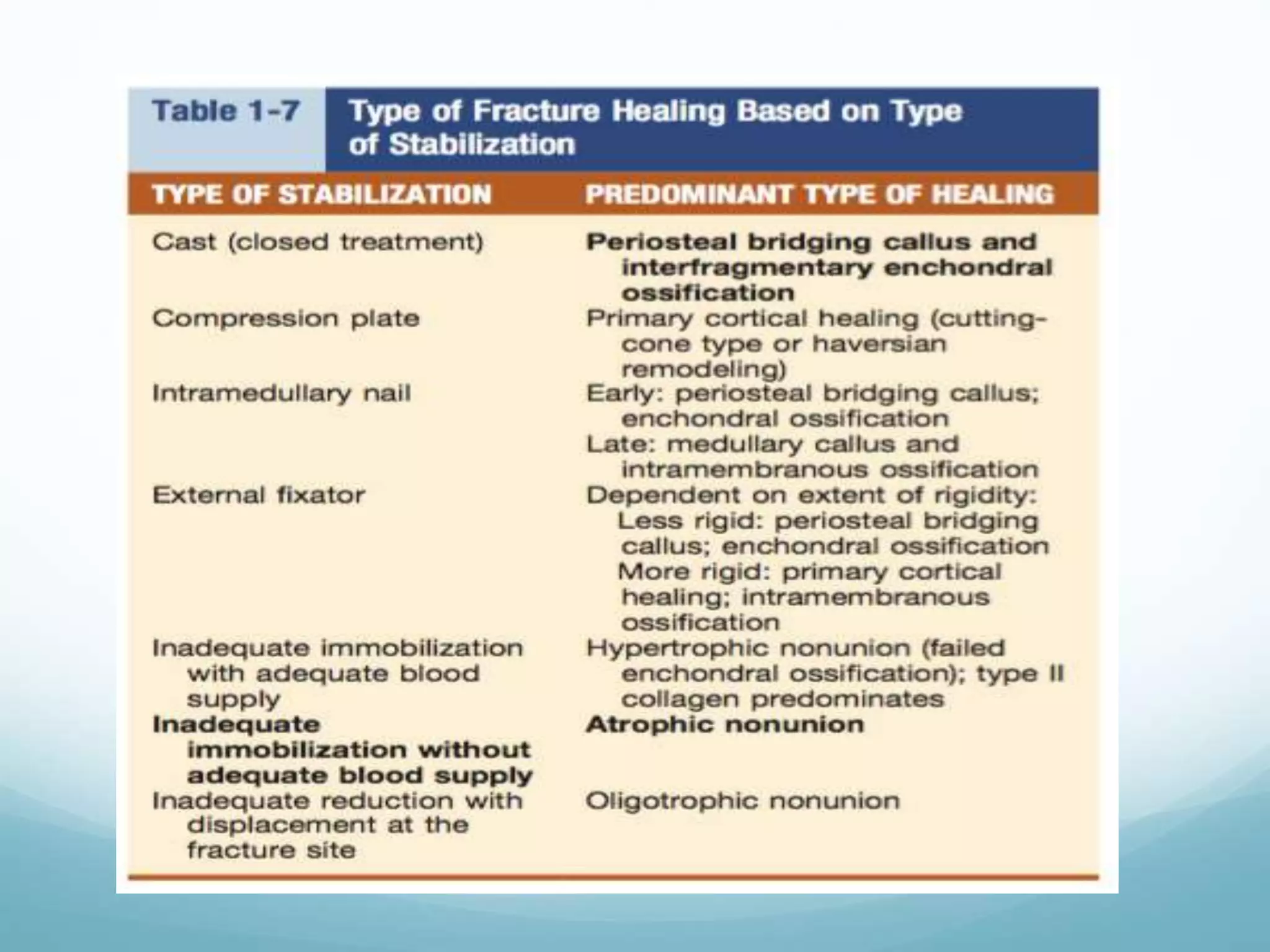
The document discusses fractures, including their classification based on various criteria such as etiology, displacement, and healing processes. It outlines the stages of fracture healing, distinguishing between primary and secondary healing, and explains the physiological requirements for effective healing. Key growth factors and the principles of stability in fracture healing are also addressed.