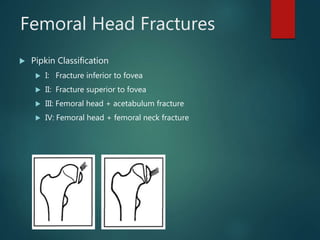
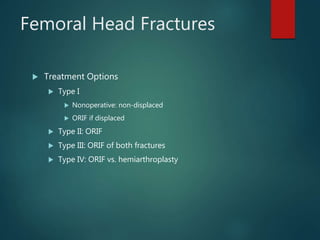
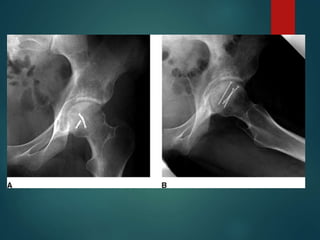
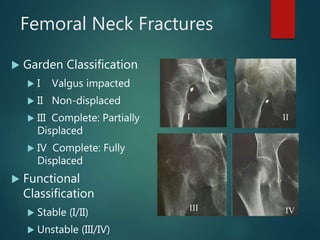
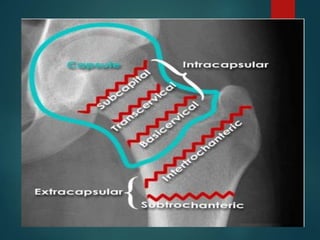
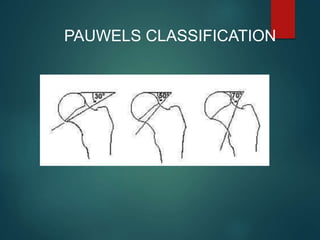
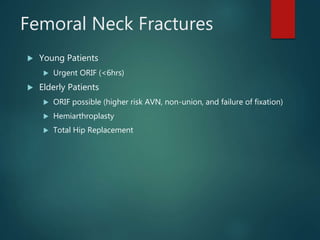
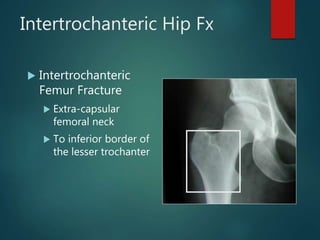
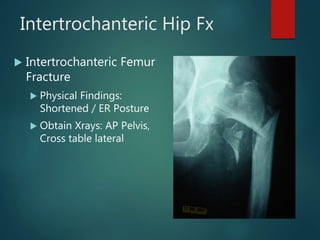
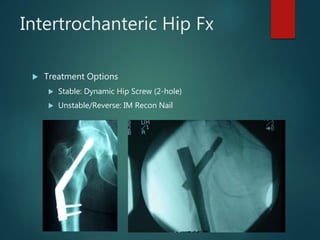
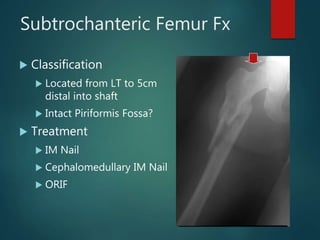
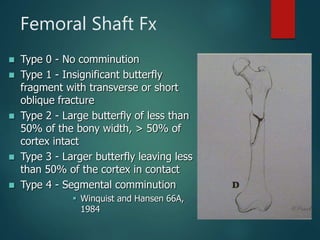
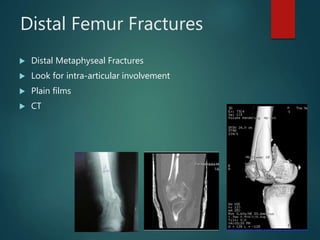
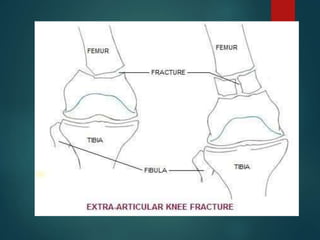
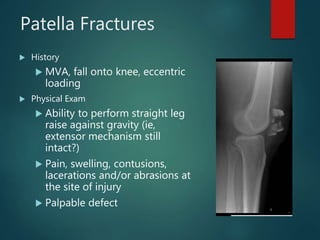
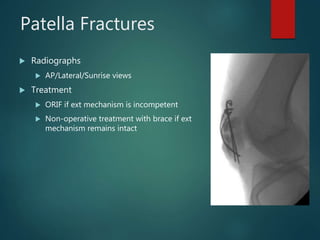
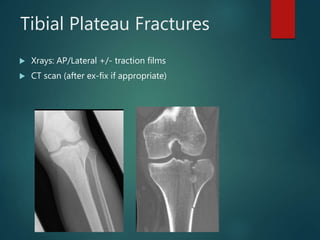
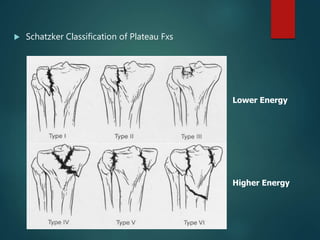
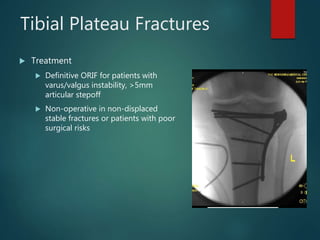
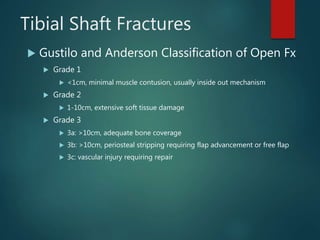
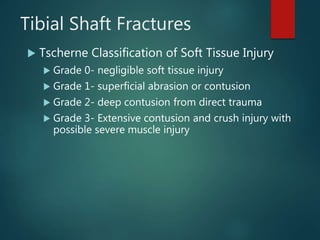
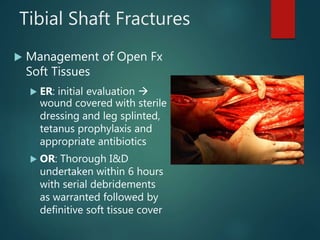
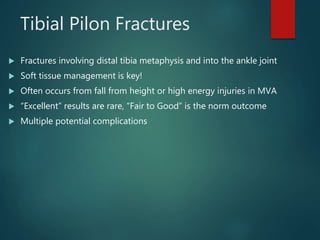
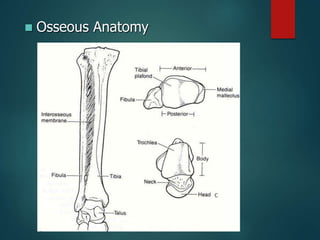
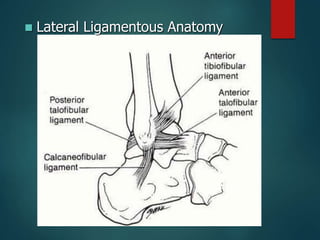
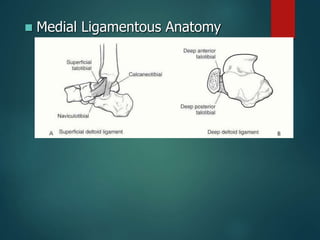
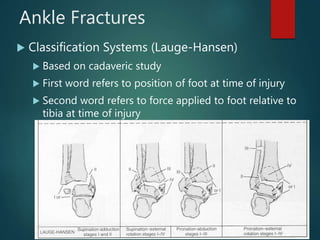
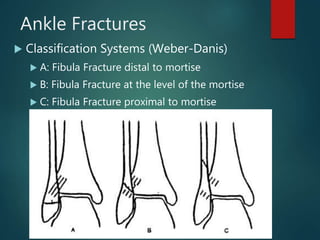
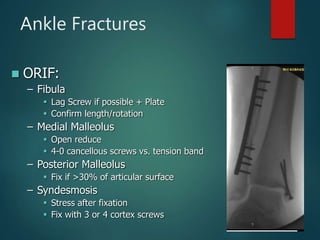
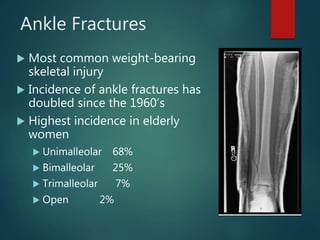
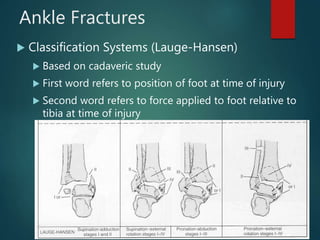
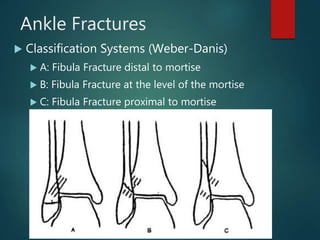
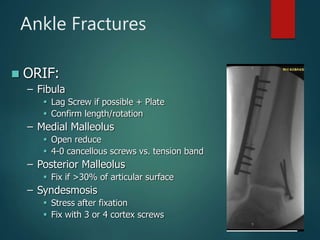
This document provides an overview of lower limb fractures, focusing on the hip, femur, knee, tibia, and ankle. It describes the epidemiology, classification systems, clinical evaluation, imaging, and treatment options for various fractures in these areas. Key points covered include the types and management of femoral neck, intertrochanteric hip, tibial plateau and pilon fractures. Evaluation involves history, exam, and radiographs, while treatment may involve fixation, arthroplasty or non-operative management depending on the fracture pattern and patient factors. Complications are also discussed for several injuries.