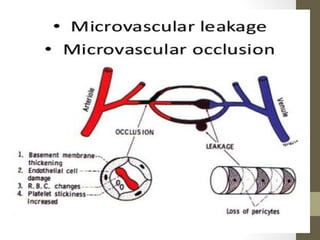
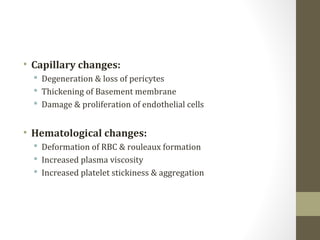
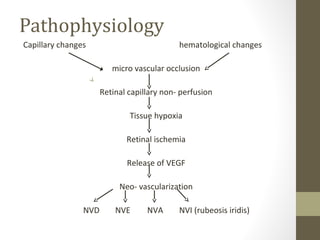
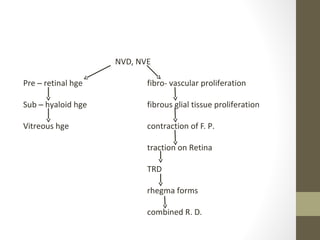
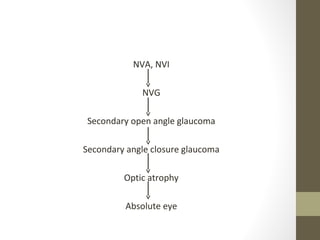
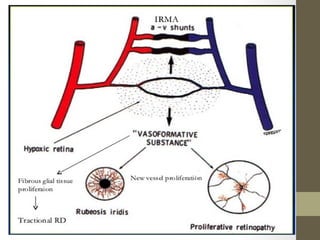
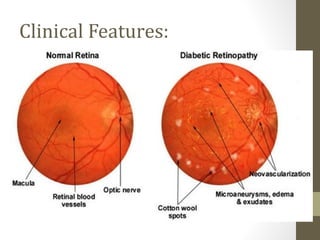
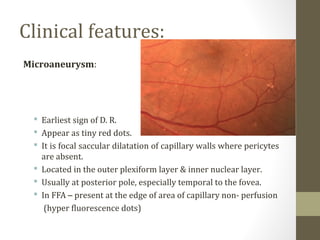
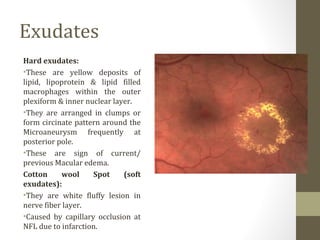
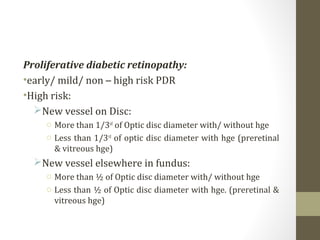
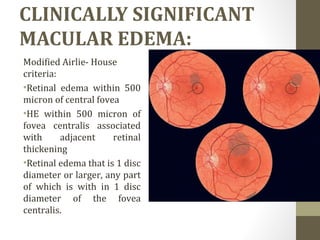
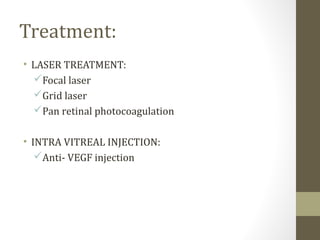
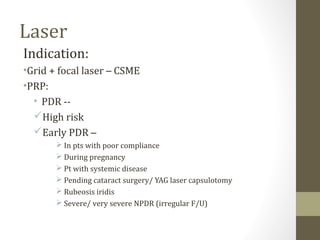
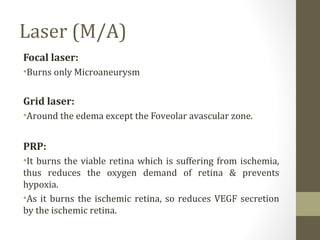
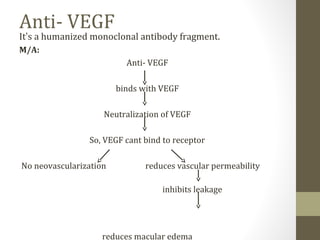
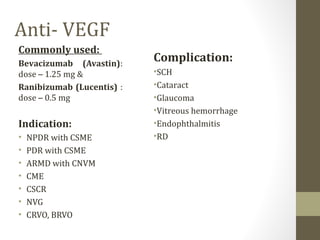
Diabetic retinopathy is a disease of the retina caused by damage to blood vessels due to long-term effects of diabetes, and is a leading cause of vision loss. It can cause microaneurysms, hemorrhages, cotton wool spots, hard exudates, and the growth of new abnormal blood vessels. Prolonged poor blood sugar control, hypertension, and other factors increase the risk. Treatment involves laser therapy such as focal laser treatment for macular edema or pan-retinal photocoagulation for proliferative retinopathy. Anti-VEGF injections are also used to treat macular edema and neovascularization by inhibiting vascular leakage and growth of abnormal vessels. Regular screening is important