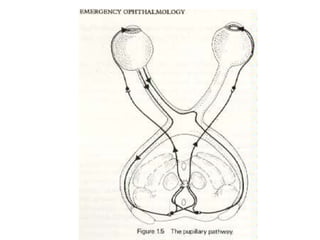
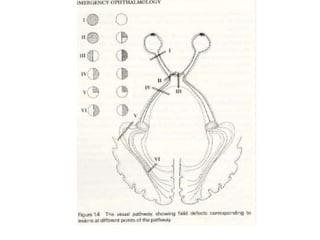
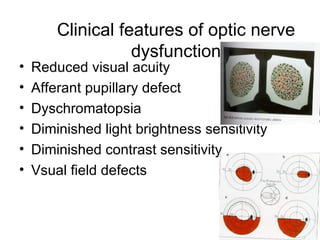
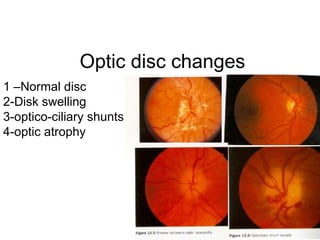
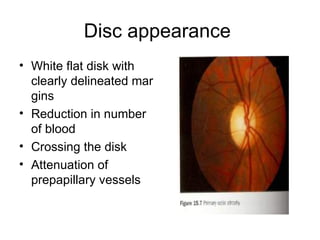
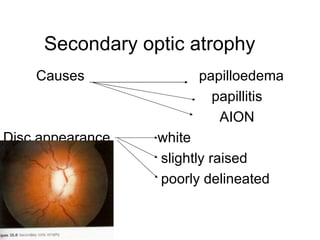
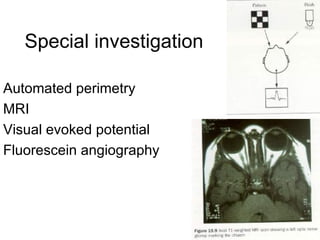
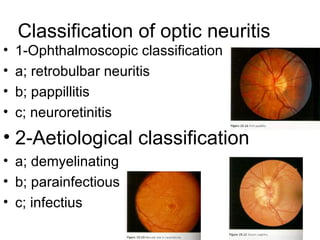
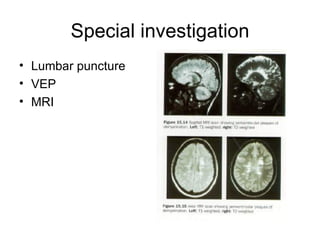
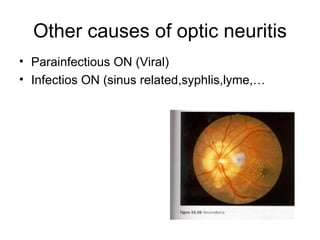
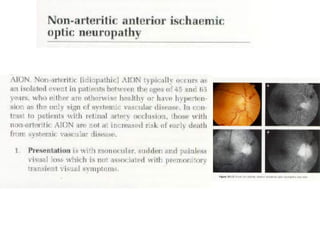
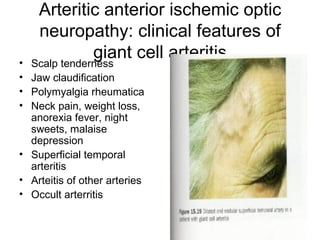
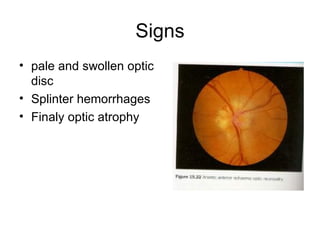
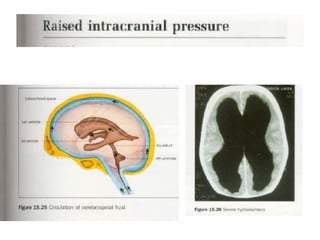
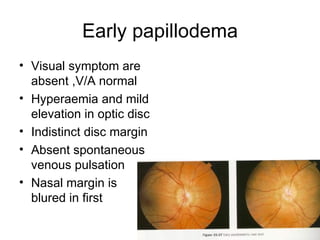
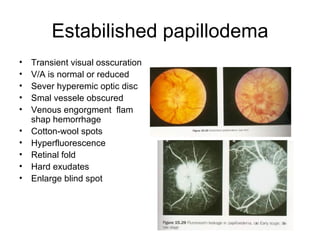
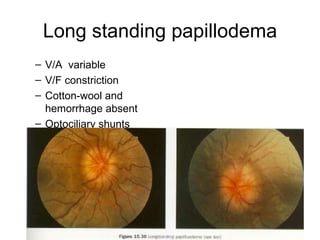
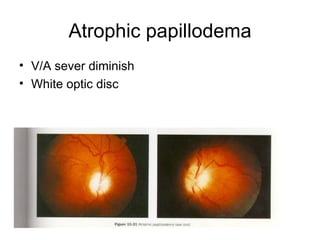
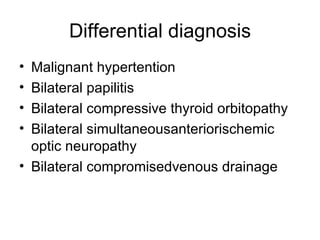
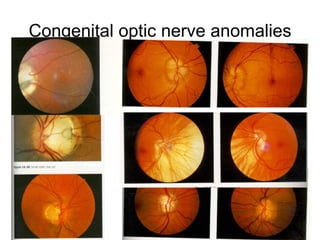
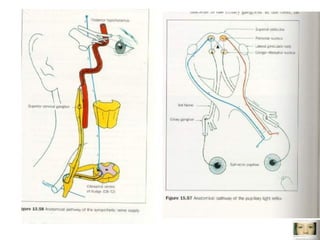
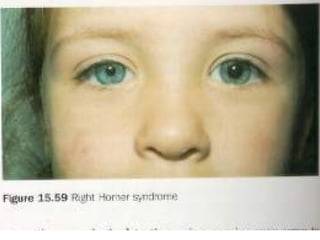
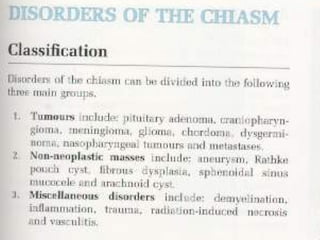
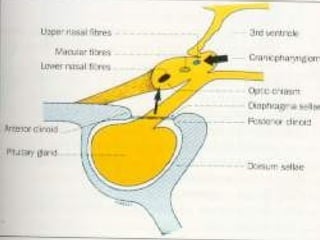
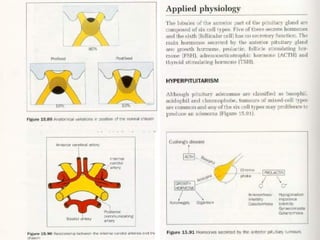
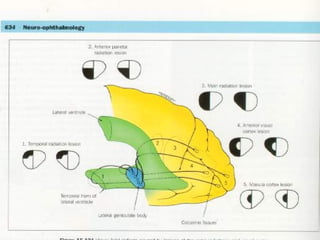
This document discusses the evaluation and classification of various optic nerve diseases. It covers clinical features of optic nerve dysfunction, optic disc changes, types of optic atrophy, signs of secondary optic atrophy, special investigations, classification of optic neuritis, associations between optic neuritis and demyelination diseases, clinical features and treatment of optic neuritis, and other causes of optic neuritis including infectious, parainfectious, and arteritic anterior ischemic optic neuropathy.