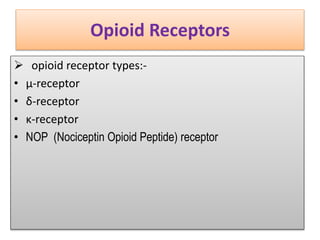
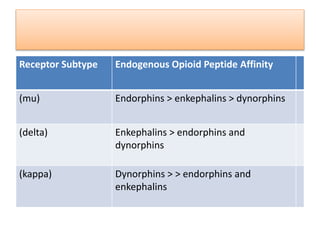
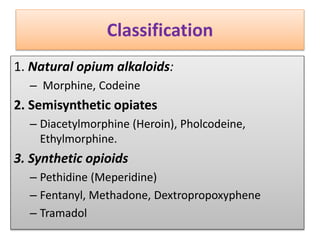
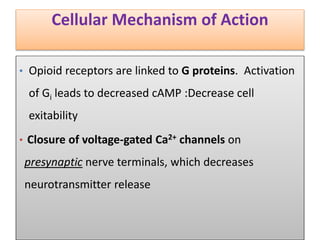
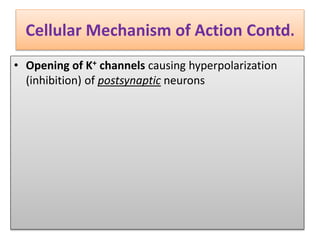
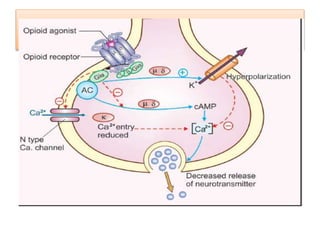
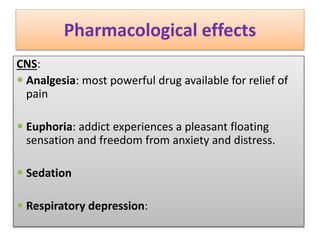
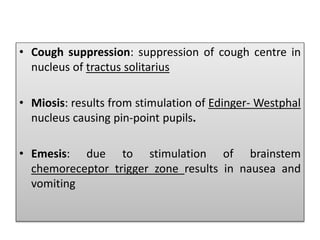
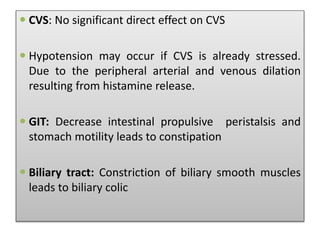
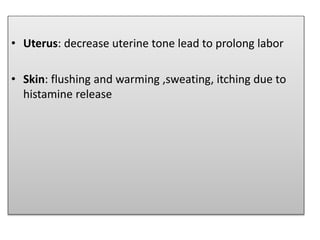
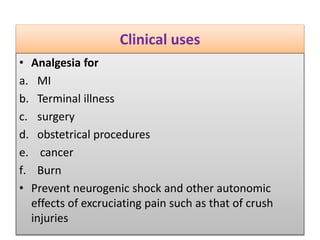
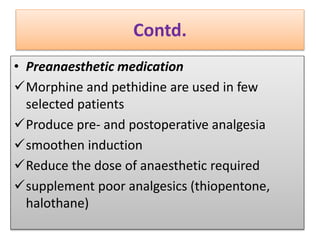
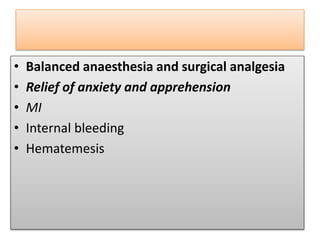
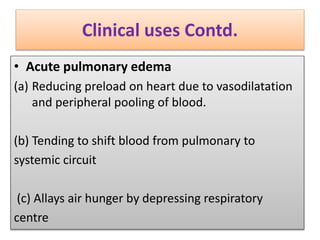
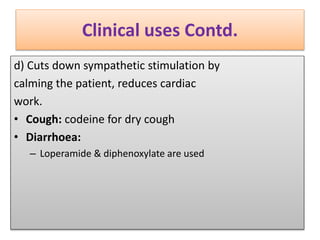
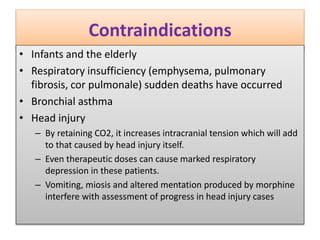
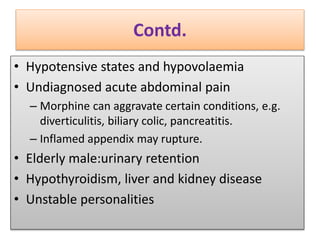
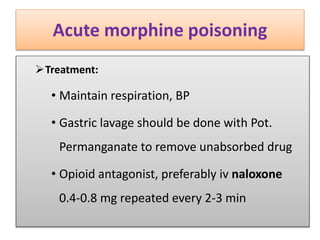
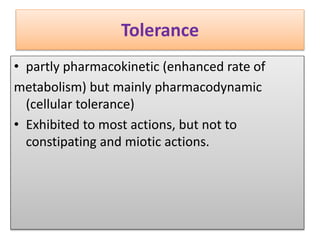
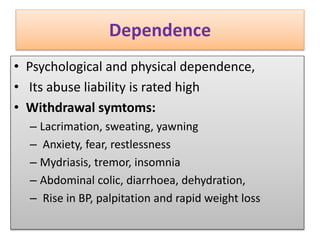
This document discusses opioid analgesics, focusing on morphine. It describes opioid receptors and their endogenous ligands. Morphine is classified as a natural opium alkaloid. Its mechanism of action involves activating Gi proteins in opioid receptors to decrease cAMP, reducing cell excitability. Clinically, morphine is used for analgesia but can cause respiratory depression, constipation, and dependence with chronic use. Dependence is treated by substituting methadone and gradually withdrawing it.