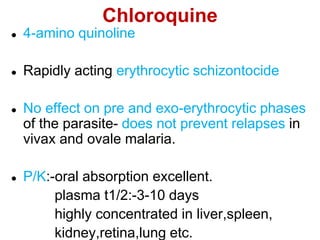
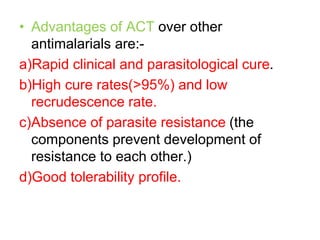
This document discusses drug therapy for malaria. It defines malaria and describes the life cycle and species of Plasmodium that cause malaria in humans. It then discusses the clinical presentation of malaria and diagnosis. The bulk of the document categorizes and describes various classes of antimalarial drugs, including quinine, chloroquine, primaquine, atovaquone, lumefantrine, and artemisinin derivatives. It provides details on the mechanisms of action, pharmacokinetics, uses, and adverse effects of many common antimalarial medications.