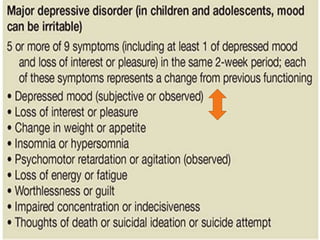
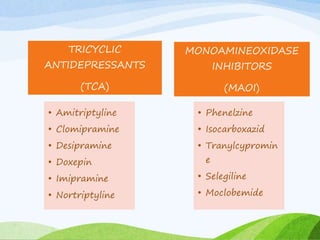
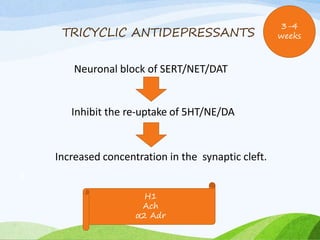
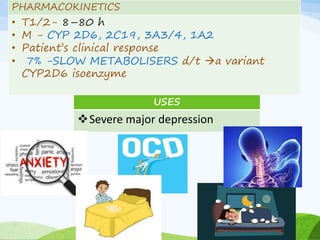
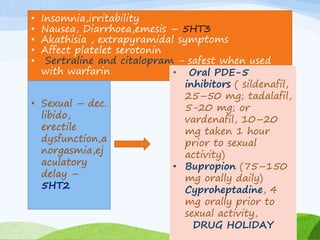
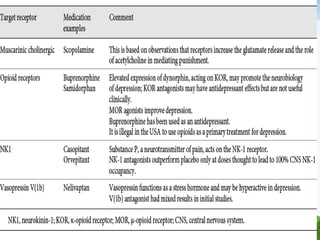
The document discusses various types of antidepressant medications, including tricyclic antidepressants, monoamine oxidase inhibitors, selective serotonin reuptake inhibitors, and newer drugs. It covers the mechanisms of action, pharmacokinetics, uses, adverse effects, and guidelines for treatment of major depressive disorder with these classes of antidepressants. Recent research into glutamatergic drugs and esketamine that target the NMDA receptor are also mentioned as promising new treatments for treatment resistant depression.



























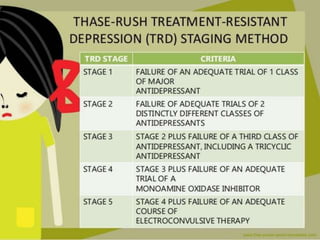
![TREATMENT
RESISTANT
DEPRESSION
The STAR*D
1. switch to a second agent that may be from the same or
different class of antidepressant
2. Augmentation with
a. Bupropion (150–450 mg/day),
b. Lithium (eg, 300–900 mg/day orally),
c. Thyroid medication (eg, liothyronine, 25–50 mcg/day
orally)
d. Second-generation antipsychotic (eg, aripiprazole [5–15
mg/day] or olanzapine [5–15 mg/day]).](https://image.slidesharecdn.com/antidepressants-190321044848/85/Antidepressants-36-320.jpg)




