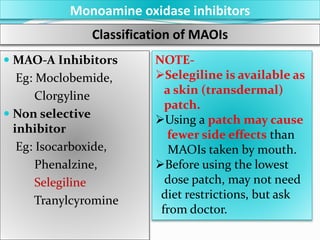
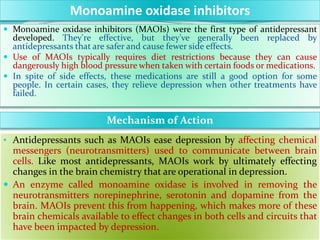
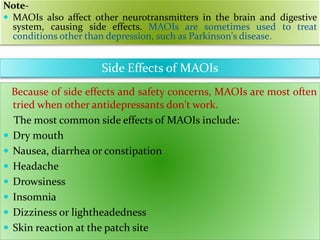
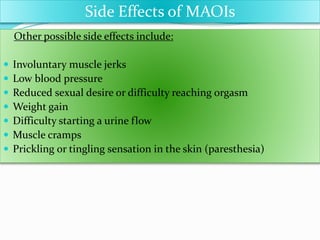
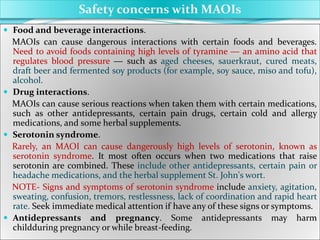
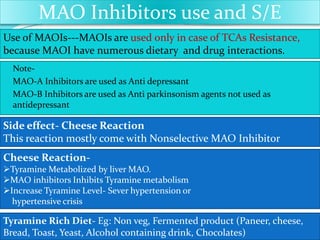
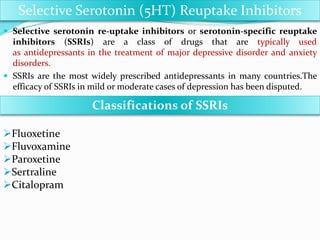
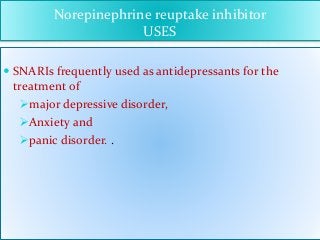
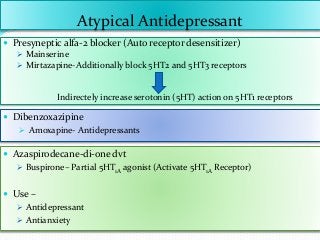
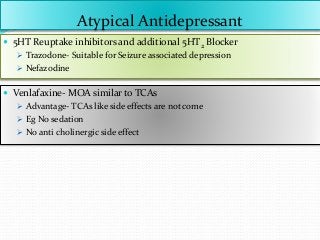
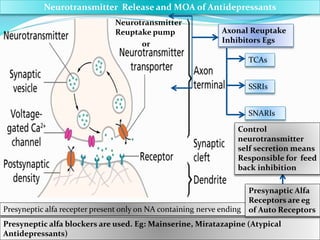
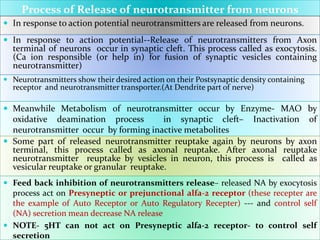
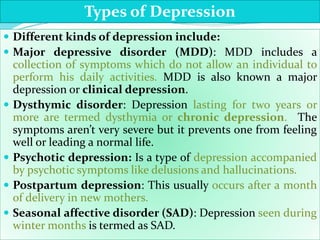
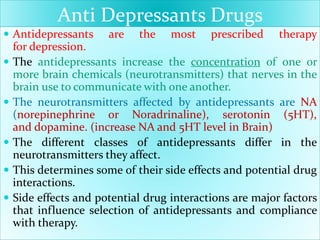
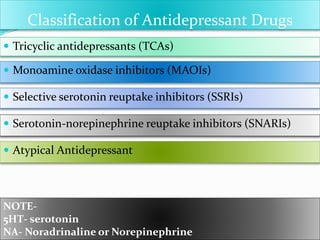
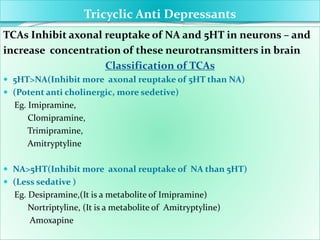
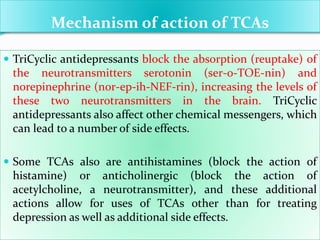
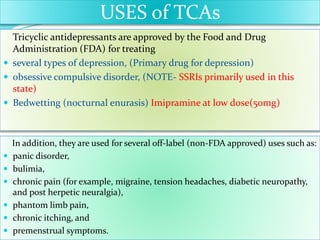
The document discusses antidepressant drugs, their mechanism of action, classifications, and the various types of depression they address. It explores neurotransmitter involvement, particularly norepinephrine and serotonin, detailing the role of tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) in treatment, along with potential side effects and drug interactions. Additionally, it emphasizes the importance of monitoring for suicidal ideation in young adults when using these medications.
![Structure and IUPAC Name of TCAs
Imipramine (IUPAC Name-
3-(10,11-dihydro-5H-dibenzo[b,f]azepin-5-
yl)-N,N-dimethylpropan-1-amine)
Trimipramine (IUPAC Name-
(±)-3-(10,11-dihydro-5H-dibenzo[b,f]azepin-5-
yl)-N,N,2-trimethylpropan-1-amine)
Amitryptyline (IUPAC Name-
3-(10,11-Dihydro-5H-dibenzo [a,d]
cycloheptene-5-ylidene)-N,N-
dimethylpropan-1-amine)
Clomipramine (IUPAC Name
3-(3-chloro-10,11-dihydro-5H-dibenzo[b,f]
azepin-5-yl)-N,N-dimethylpropan-1-amine)](https://image.slidesharecdn.com/antidepressants-160705124708/85/Antidepressants-12-320.jpg)
![Structure and IUPAC Name of TCAs
Desipramine (IUPAC Name-
3-(10,11-Dihydro-5H-dibenzo[b,f]azepin-5-
yl)-N-methylpropan-1-amine
Nortriptyline (IUPAC Name-
3-(10,11-Dihydro-5H-dibenzo [a,d]
cyclohepten-5-ylidene)-N-methyl-1-
propanamine
Amoxapine (IUPAC Name-
2-chloro-11-(piperazin-1-yl) dibenzo [b,f]
[1,4]oxazepine)](https://image.slidesharecdn.com/antidepressants-160705124708/85/Antidepressants-13-320.jpg)