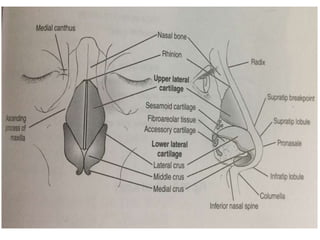
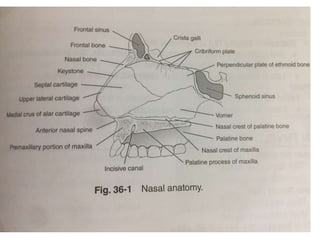
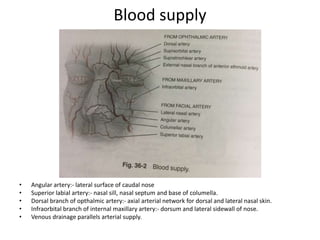
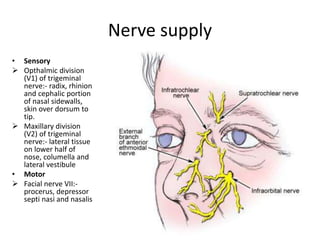
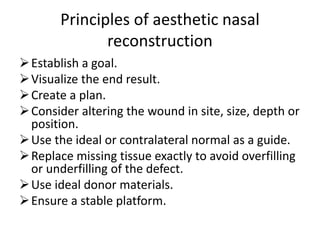
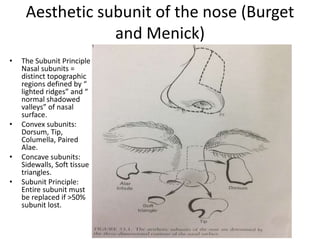
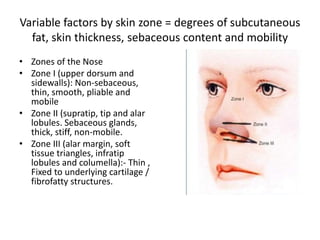
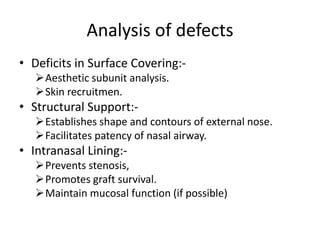
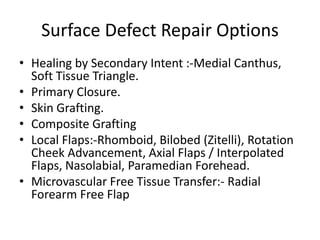
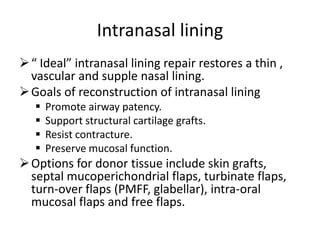
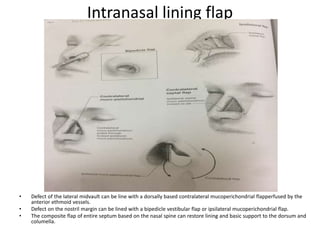
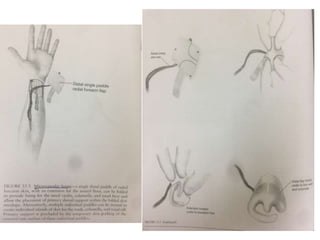
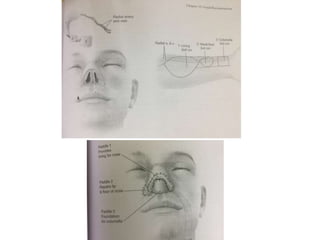
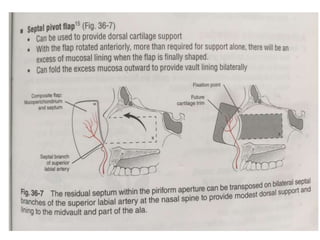
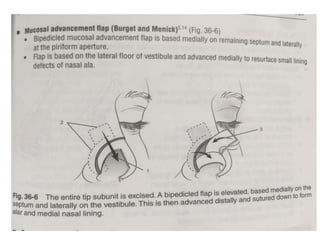
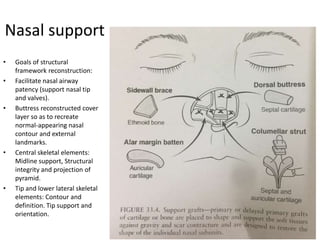
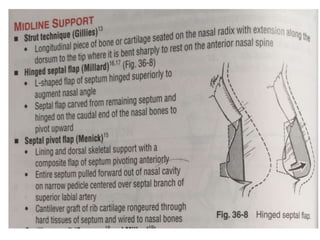
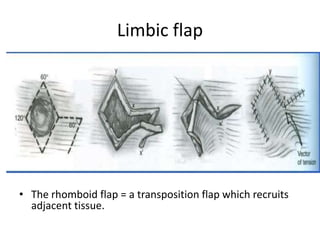
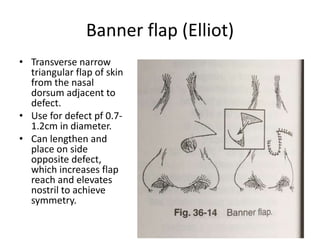
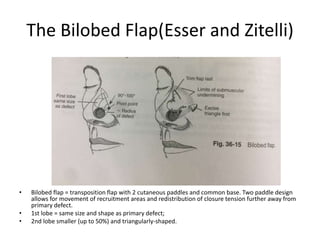
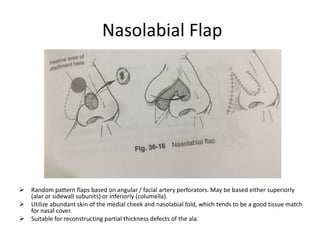
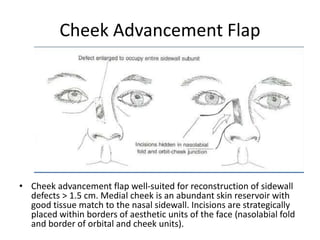
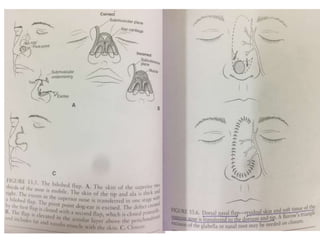
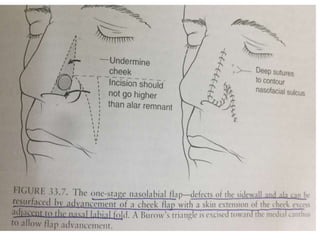
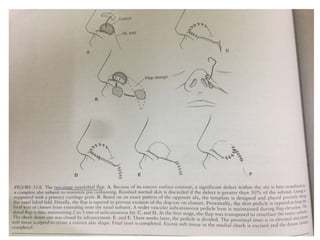
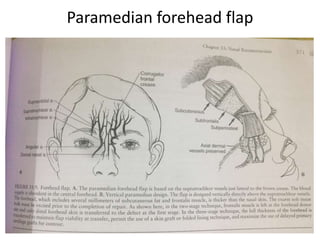
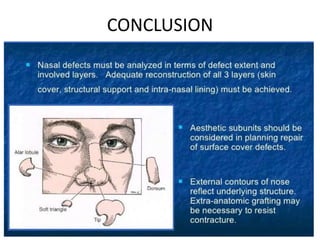
This document discusses nose reconstruction techniques. It begins by describing the anatomy and blood supply of the nose. It then discusses the nerve supply and history of nose reconstruction. Various principles and approaches to reconstruction are outlined, including analyzing defects, goals of reconstruction, and options for repairing surface defects, intranasal lining, and providing nasal support. Reconstructive techniques discussed include skin grafting, local flaps like rhomboid and bilobed flaps, and free tissue transfer. Goals are complete reconstruction while minimizing morbidity and optimizing aesthetics.