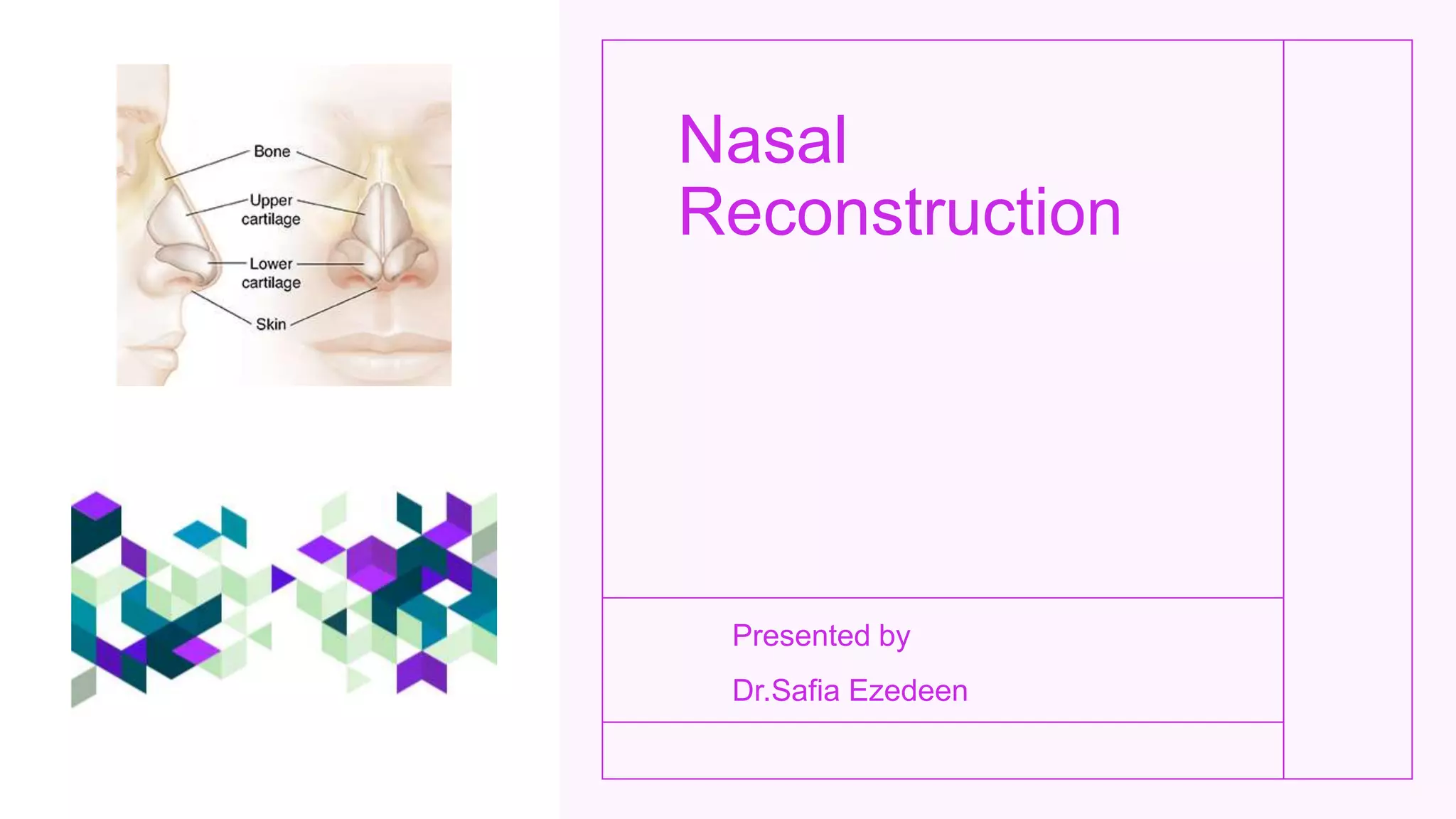
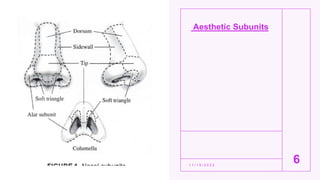
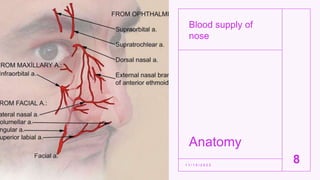
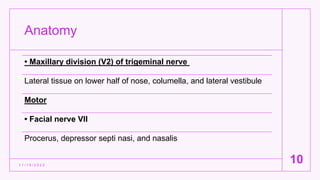
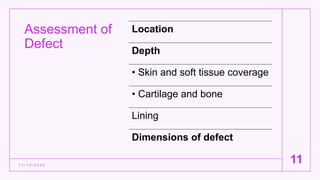
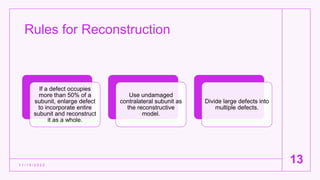
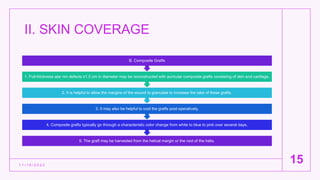
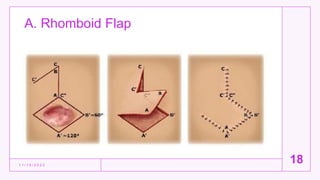
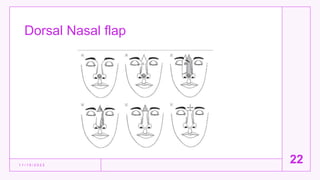
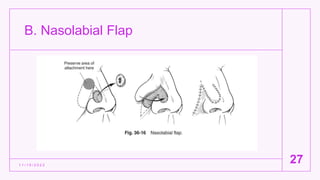
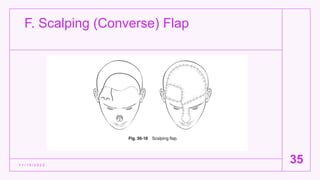
The document provides an overview of nasal reconstruction techniques, detailing the anatomy, blood supply, innervation, and various surgical options, including local and distant tissue flaps. Key goals of reconstruction include maintaining airway patency, optimizing aesthetics, and minimizing morbidity. The document emphasizes the importance of skeletal support in nasal reconstruction, outlining different graft types and techniques to achieve successful outcomes.