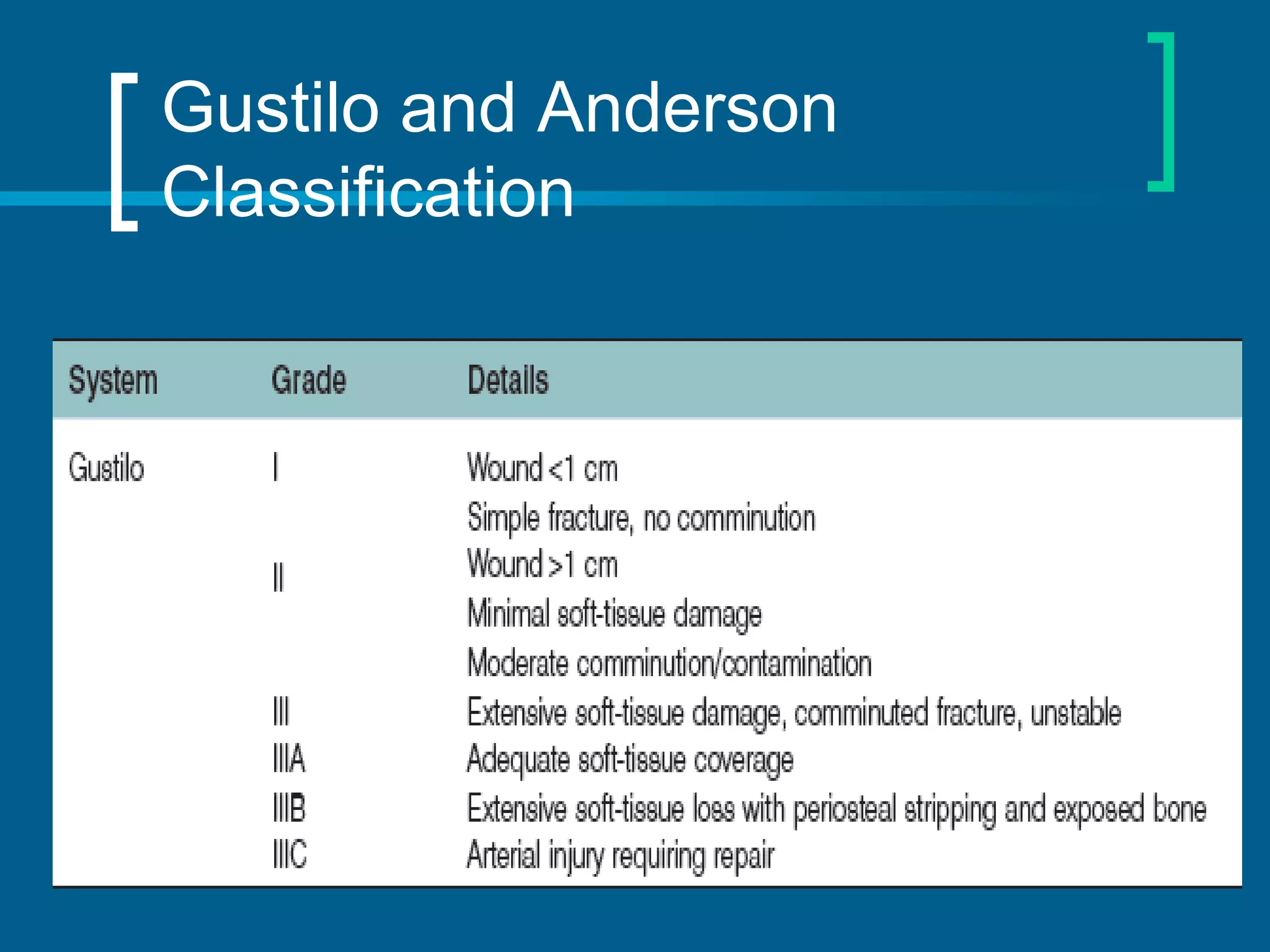
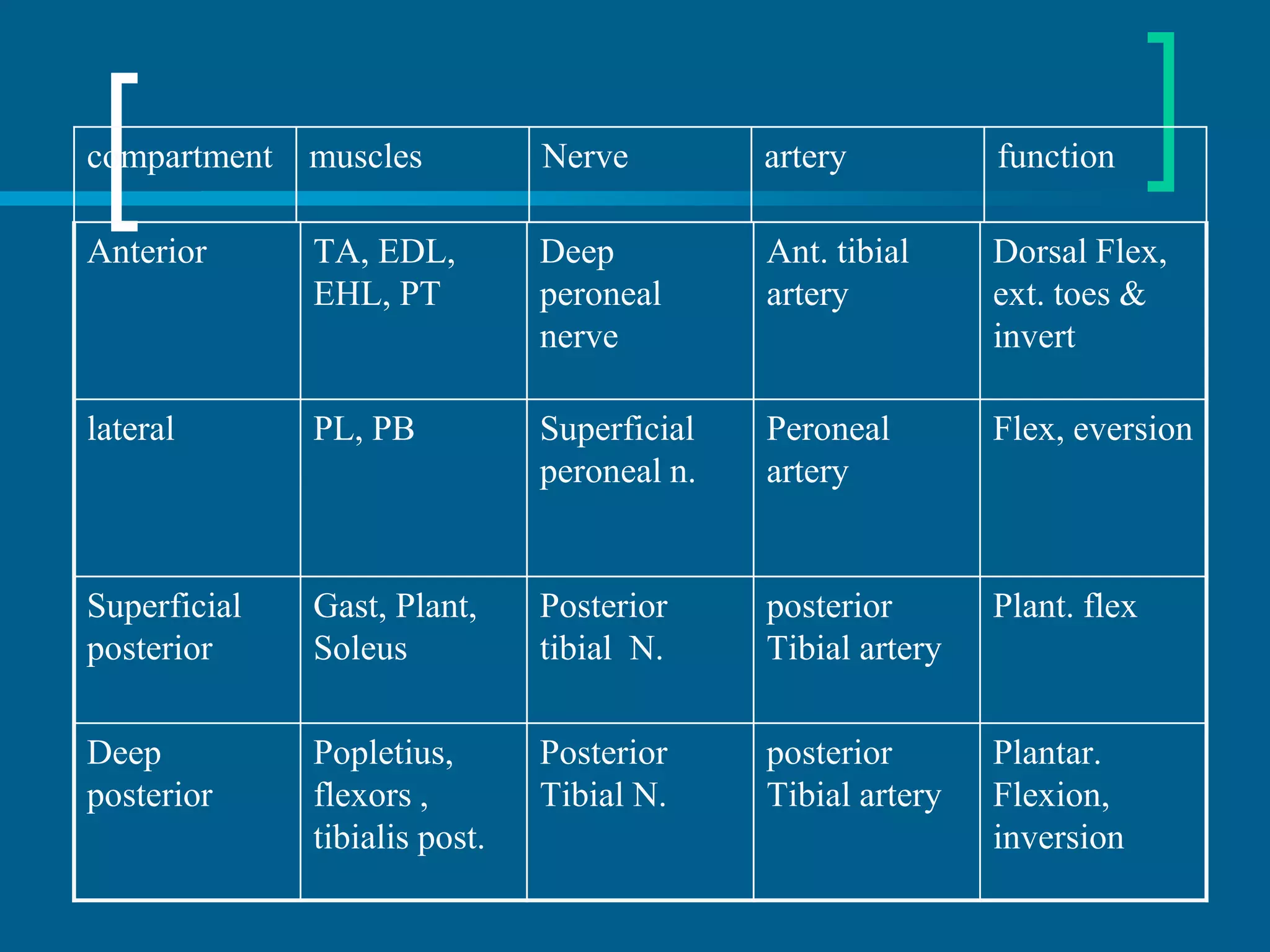
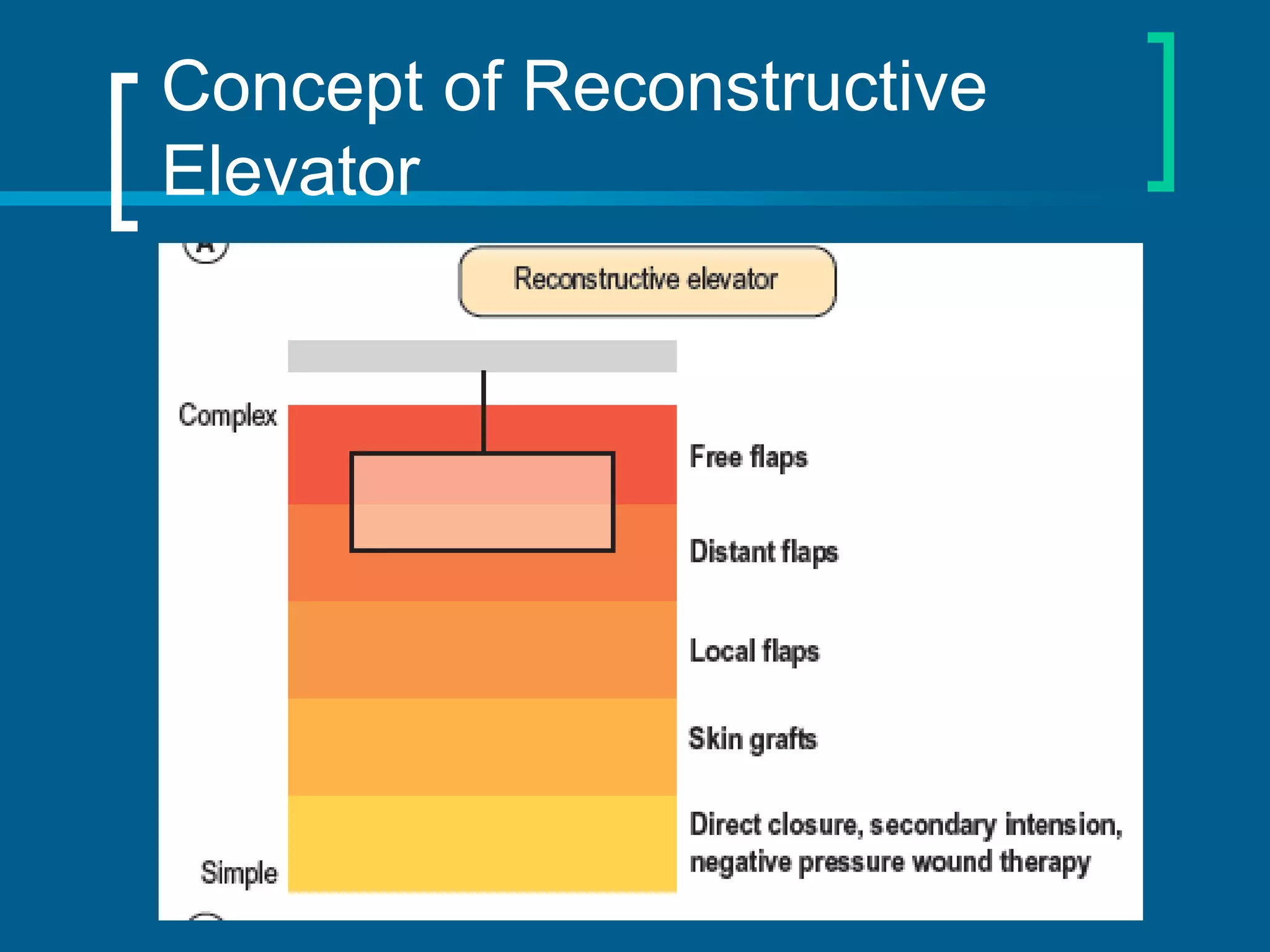
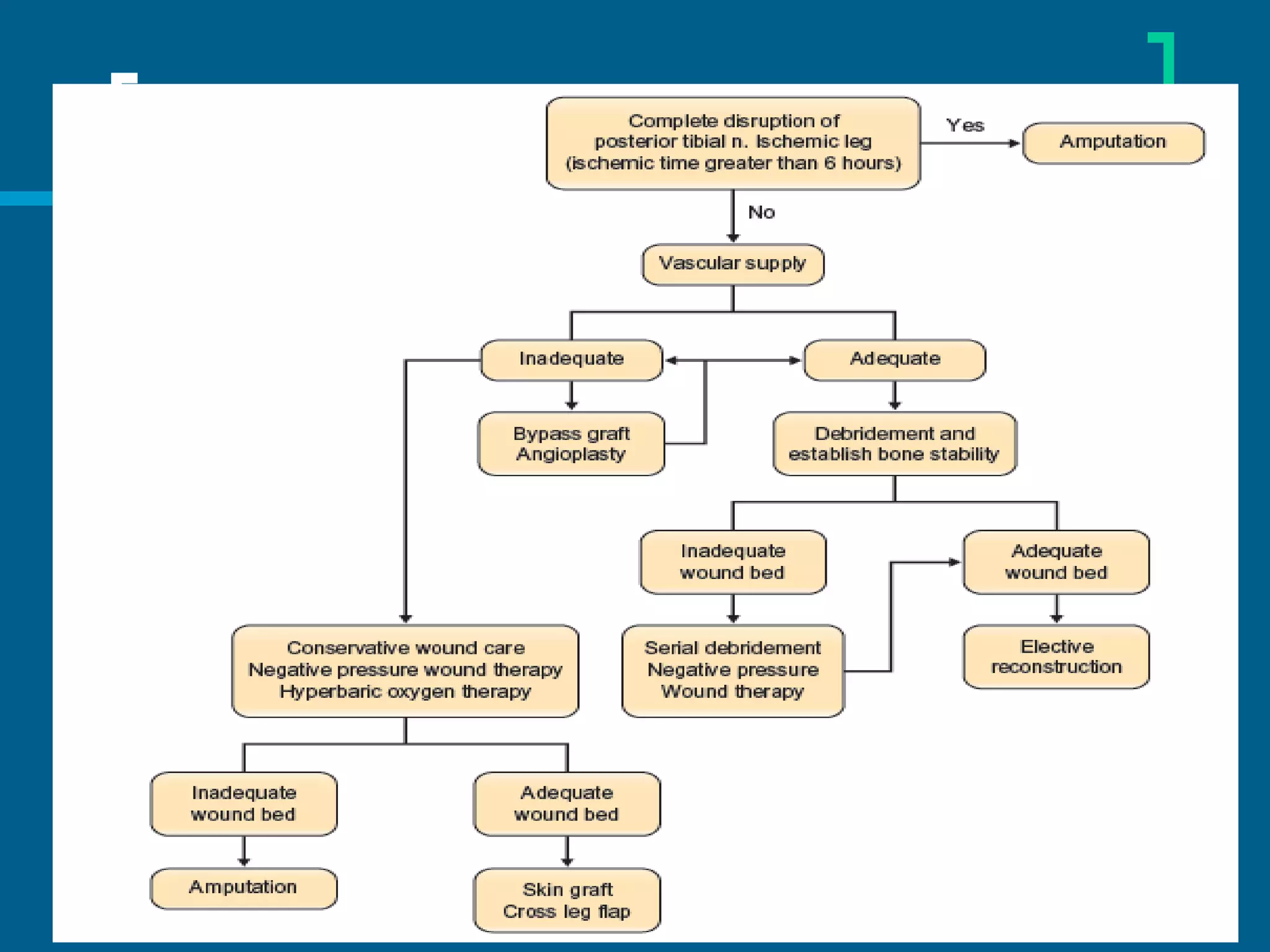
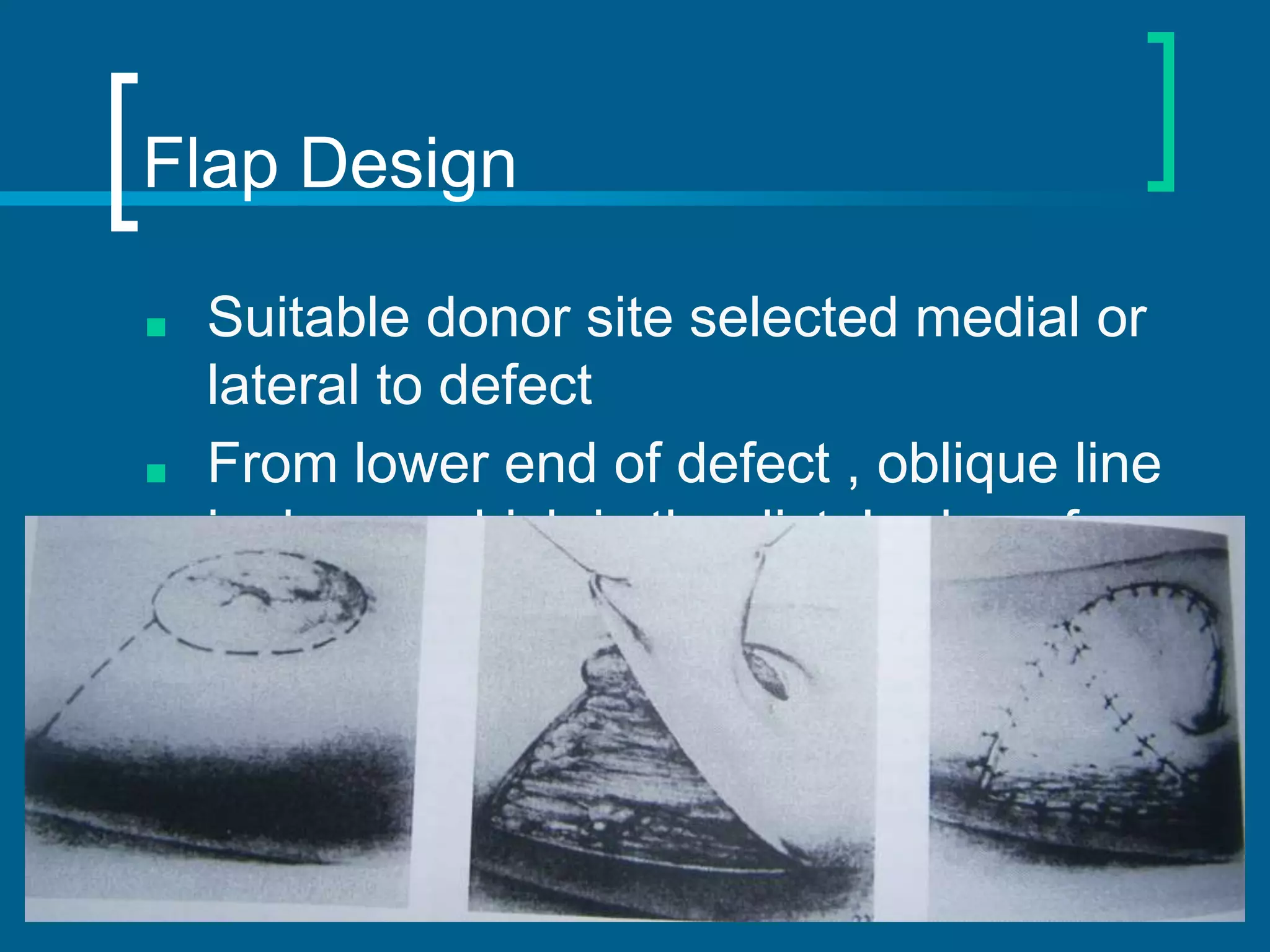
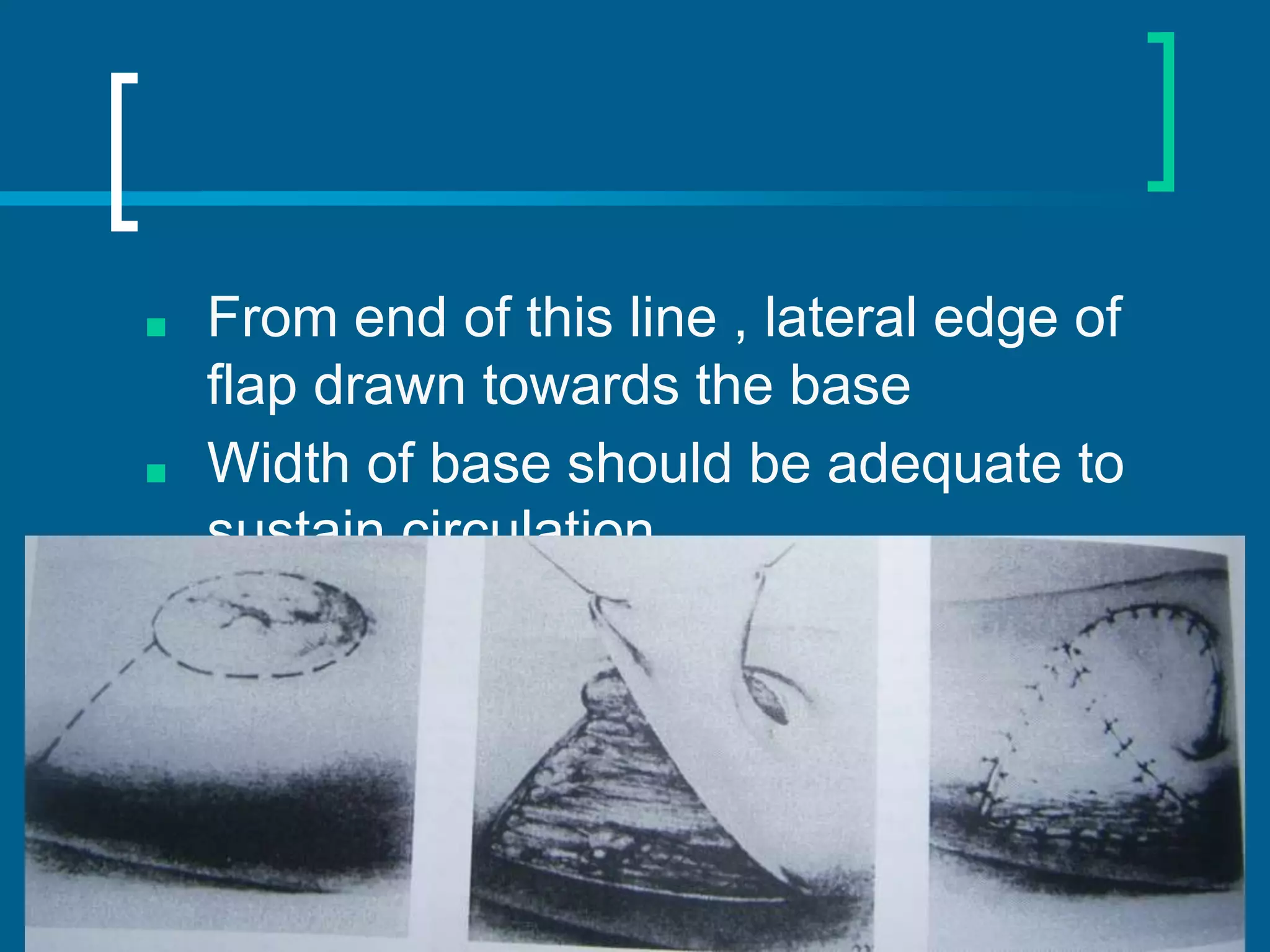
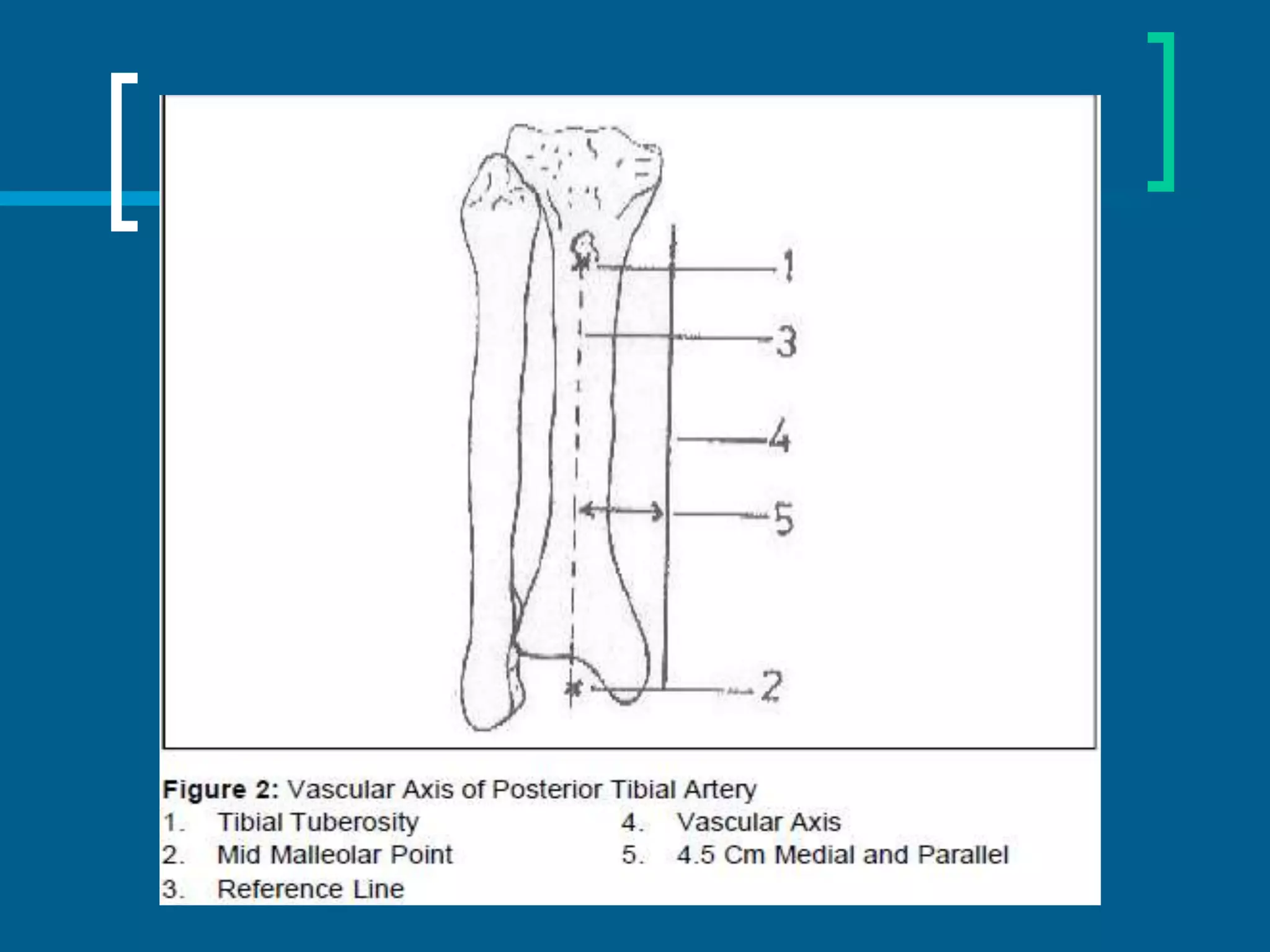
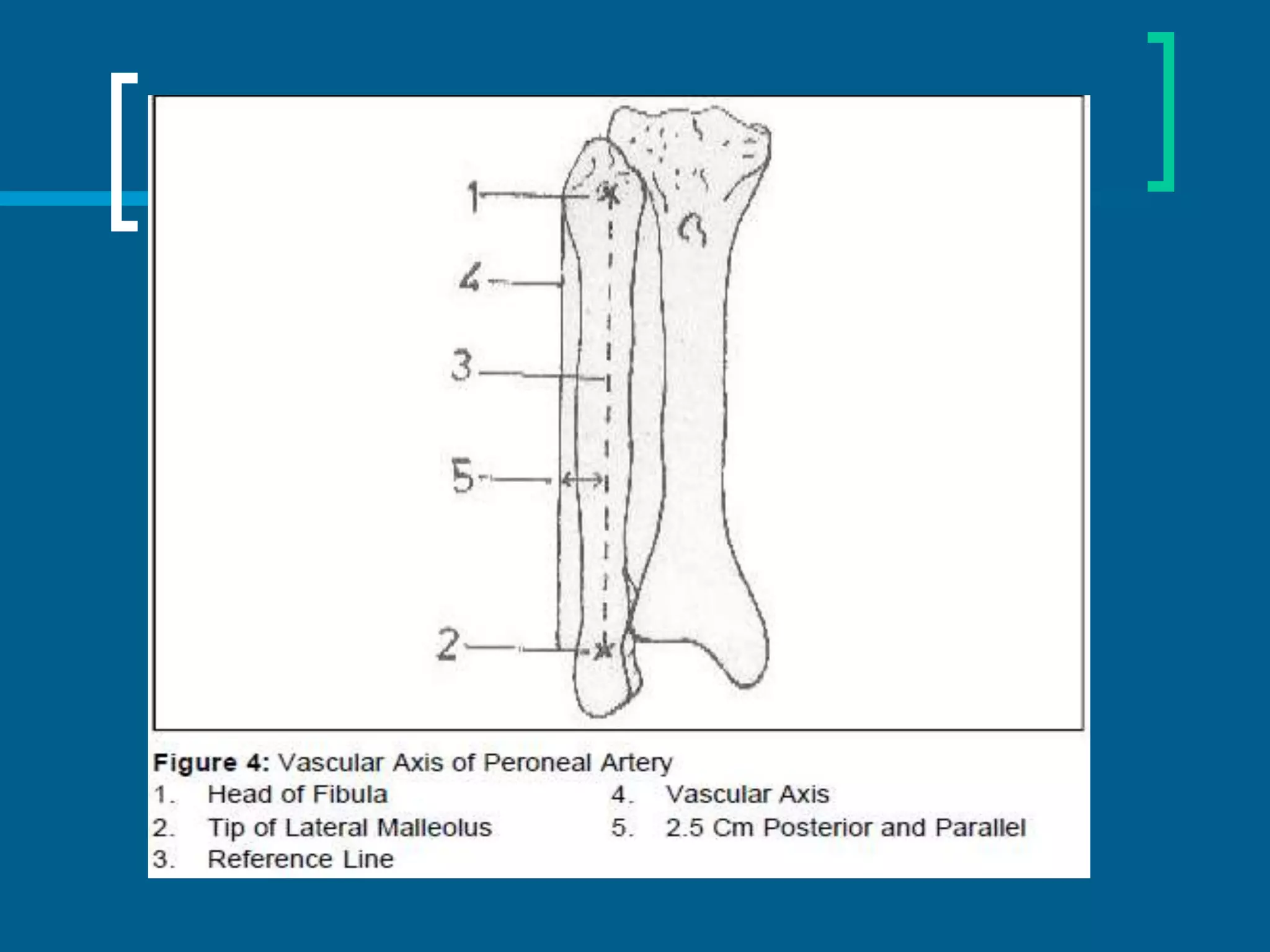
Dr. Raghav Shrotriya discusses the reconstruction techniques for upper and middle leg defects, emphasizing the importance of early intervention to minimize complications. The document outlines various criteria for amputation versus limb salvage, along with detailed approaches to wound coverage using different types of flaps and grafts. Key considerations include the patient's condition, timing of intervention, and the nature of the defects sustained from trauma or other factors.