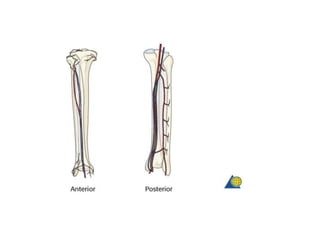
The free fibula flap technique involves harvesting a skin paddle and segment of the fibula bone based on a vascular pedicle from the peroneal artery. Key steps include:
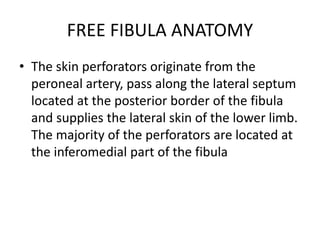
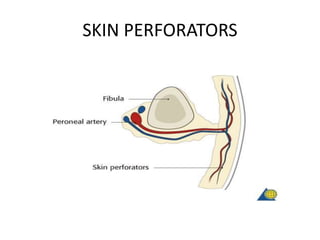
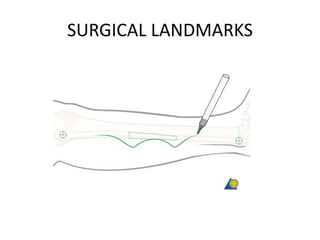
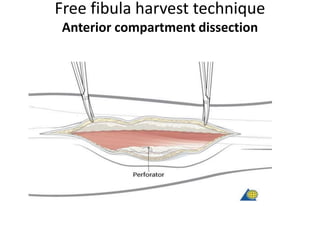
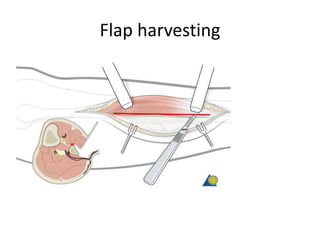
1. Identifying perforators from the peroneal artery to the skin and outlining a skin paddle.
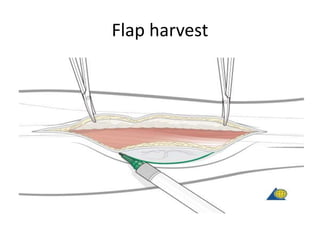
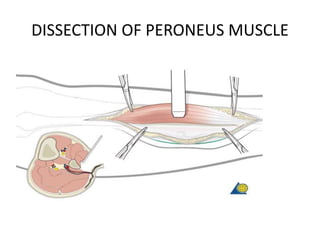
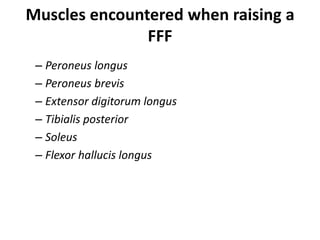
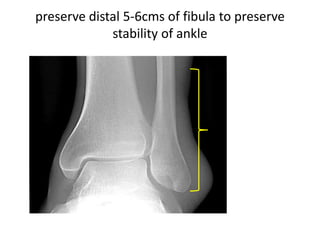
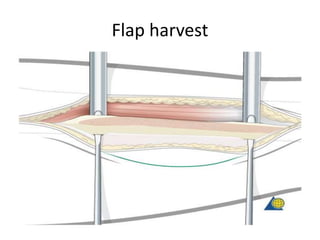
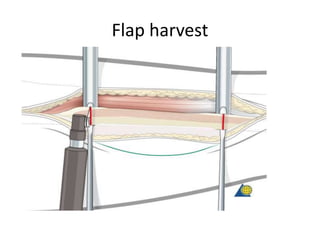
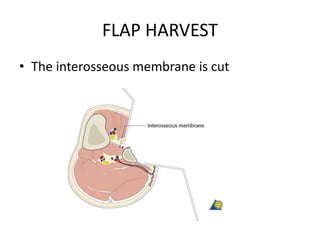
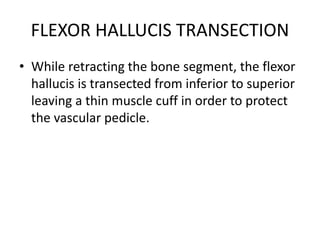
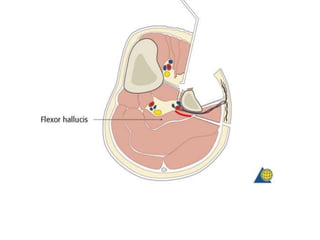
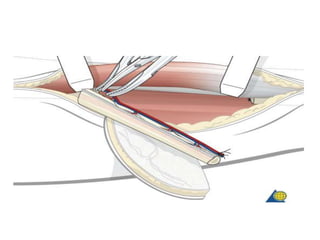
2. Elevating muscles from the fibula bone and performing osteotomies to harvest the fibula segment.
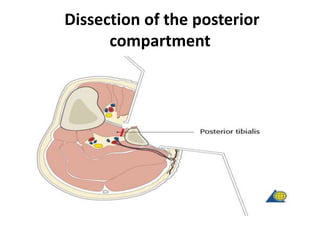
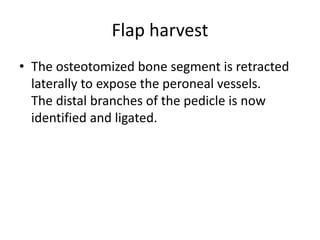
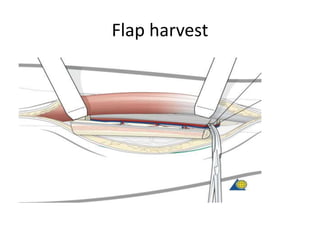
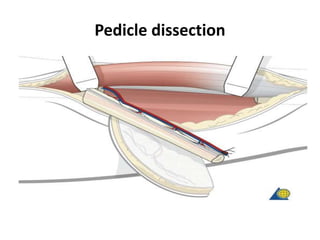
3. Dissecting the peroneal artery and its branches to isolate the vascular pedicle.
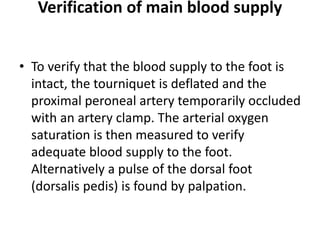
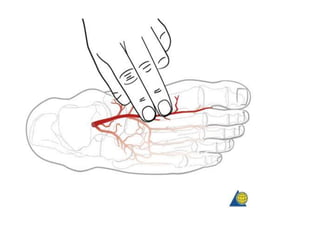
4. Verifying adequate blood flow to the foot before transecting the pedicle to the desired length.