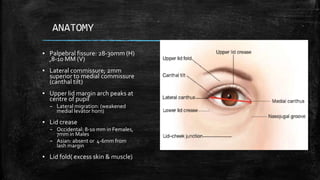
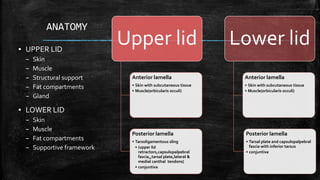
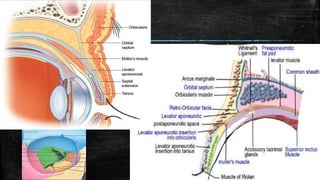
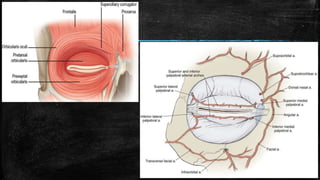
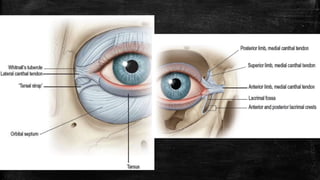
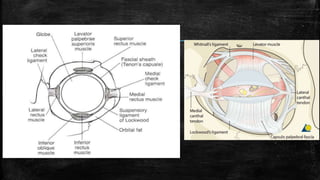
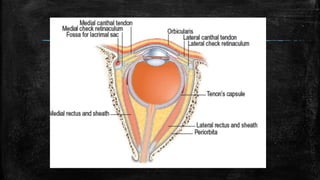
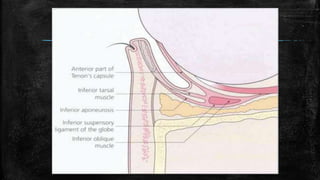
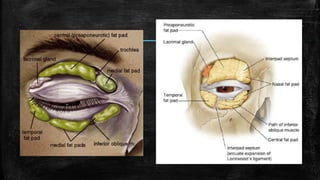
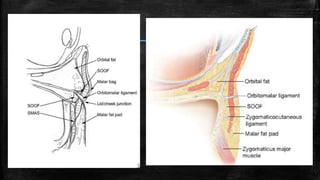
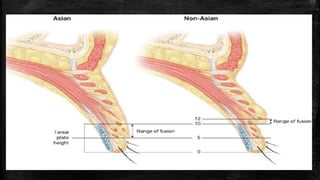
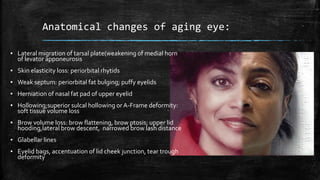
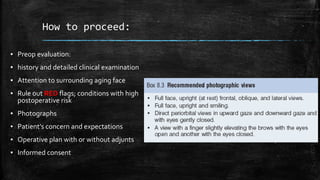
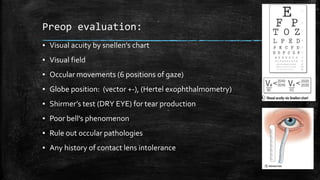
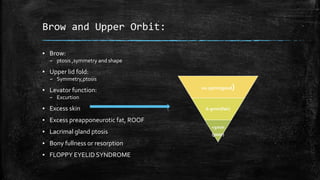
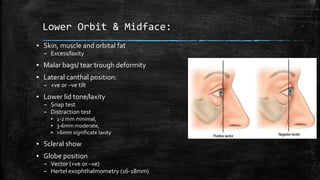
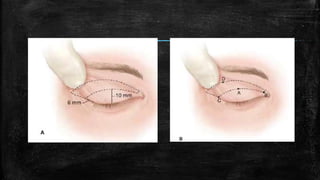
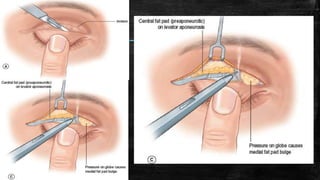
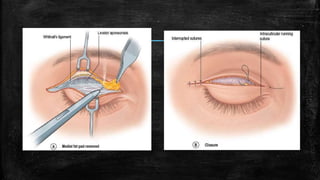
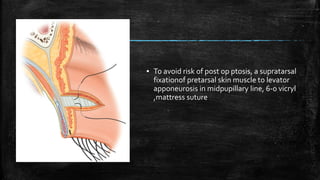
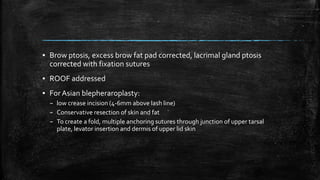
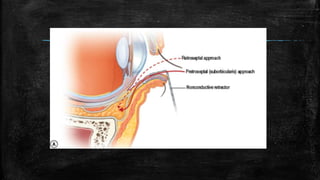
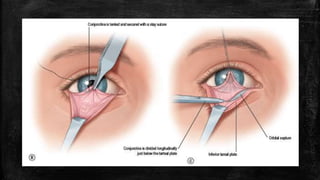
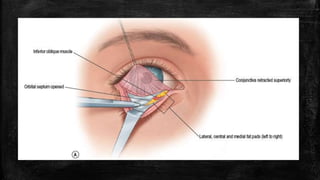
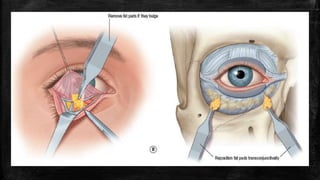
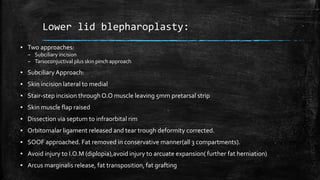
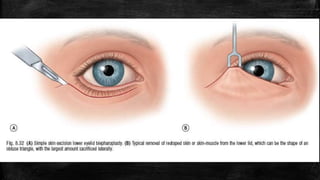
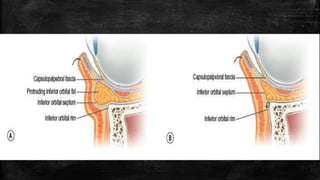
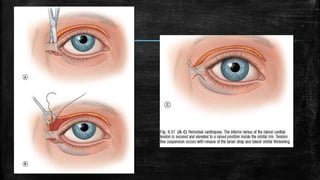
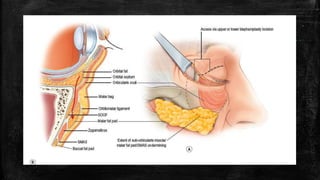
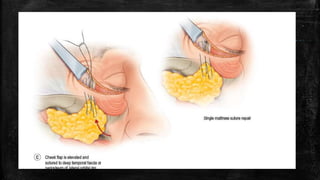
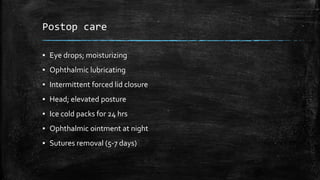
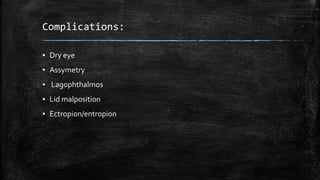
This document discusses blepharoplasty surgery to rejuvenate the upper and lower eyelids. It covers the goals of maintaining a youthful eyelid shape and position. The principles of the surgery include properly positioning the brows, restoring tone and position of the lateral canthal area and lower lids, and preserving skin, muscle and fat. It describes the anatomical changes that occur with aging around the eyes and indications for surgery. Pre-operative evaluation and different surgical techniques for the upper and lower lids are outlined, along with potential complications.