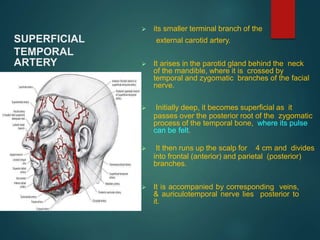
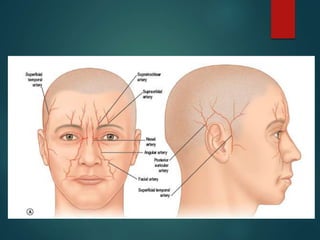
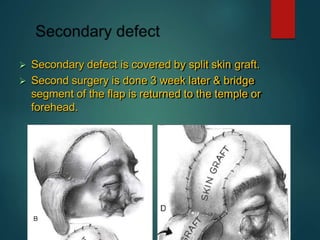
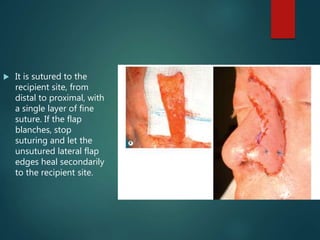
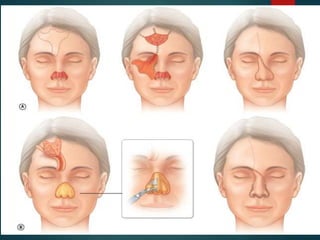
The forehead flap is a versatile flap used for reconstructing various facial defects. It has reliable blood supply from branches of the superficial temporal artery. The flap can be raised in different planes and tunneled to reach intraoral defects. It is commonly used in a two-stage procedure for nasal reconstruction, where the flap is first transferred to the defect and then the pedicle is divided later. Pre-expansion of the donor site can increase the available skin but comes with disadvantages like delaying the repair.