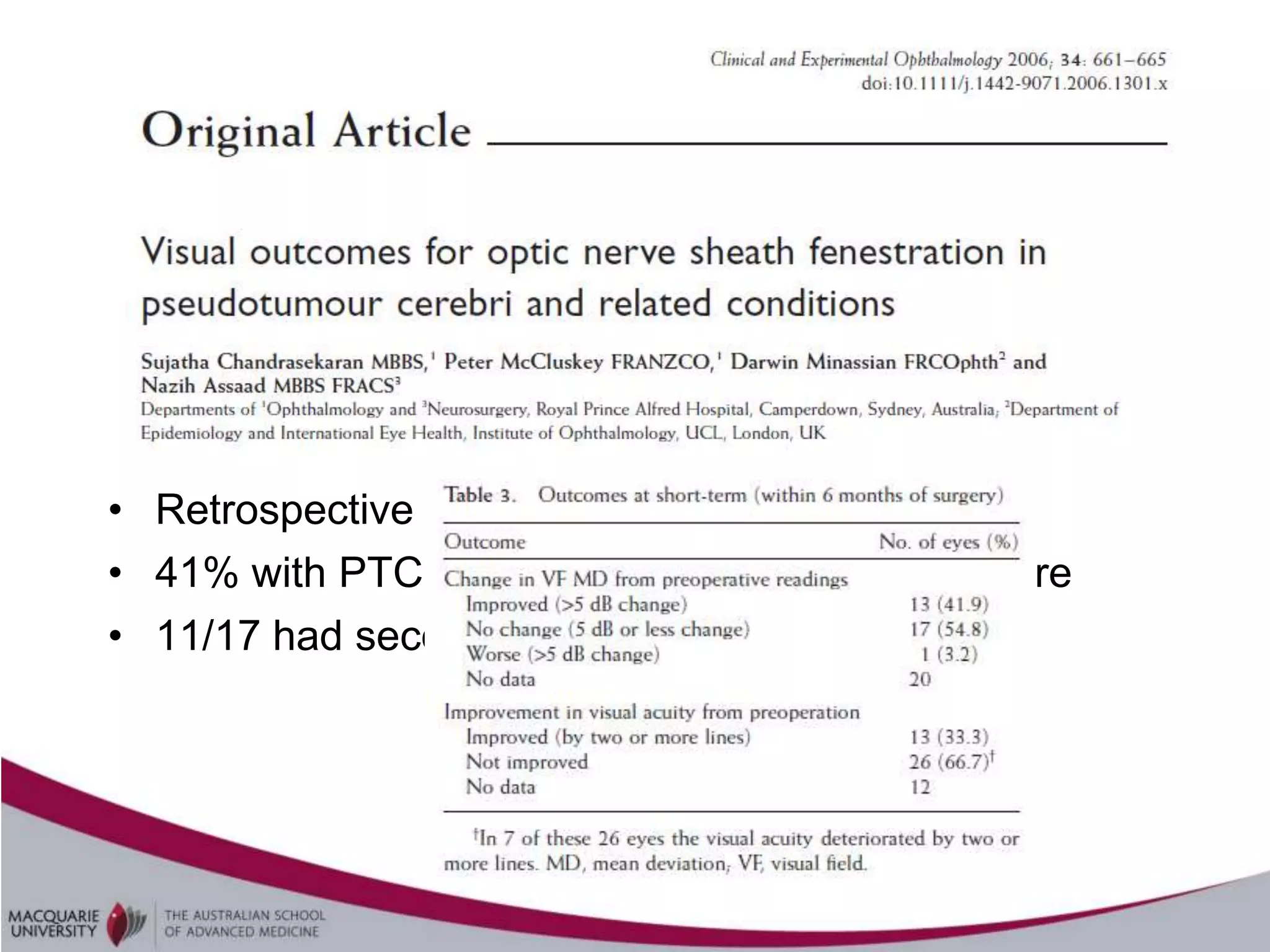
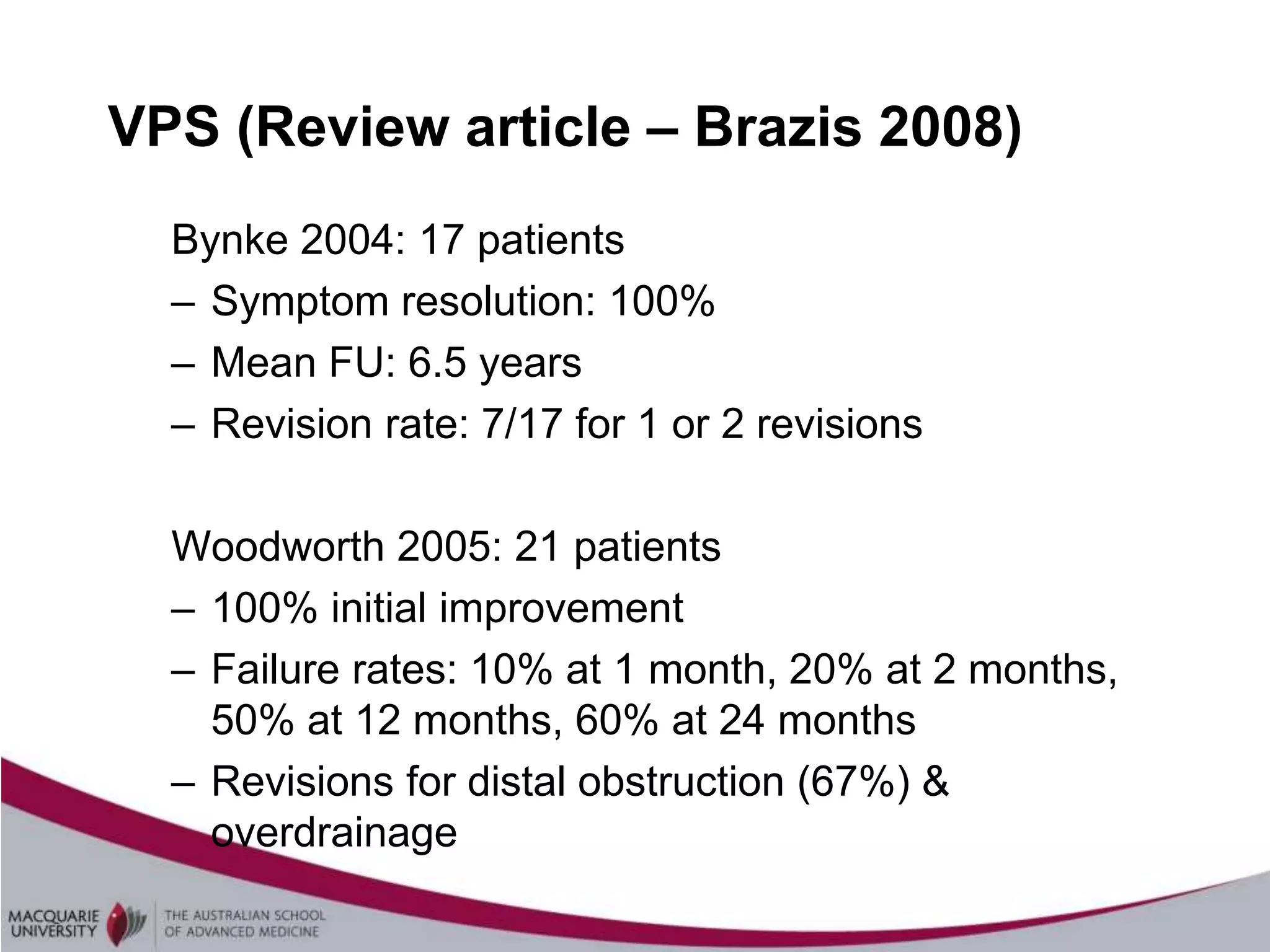
The document summarizes research on the effectiveness of optic nerve sheath fenestration (ONSF) for treating idiopathic intracranial hypertension. Case series show that ONSF is effective in the short term for resolving papilloedema and preventing visual deterioration in 85-94% of patients, though not as effective for headaches. While unilateral ONSF may be sufficient, long-term recurrence is common. ONSF appears similarly effective as lumbar punctures or ventriculoperitoneal shunts, though randomized controlled trials are still needed to determine best treatment.


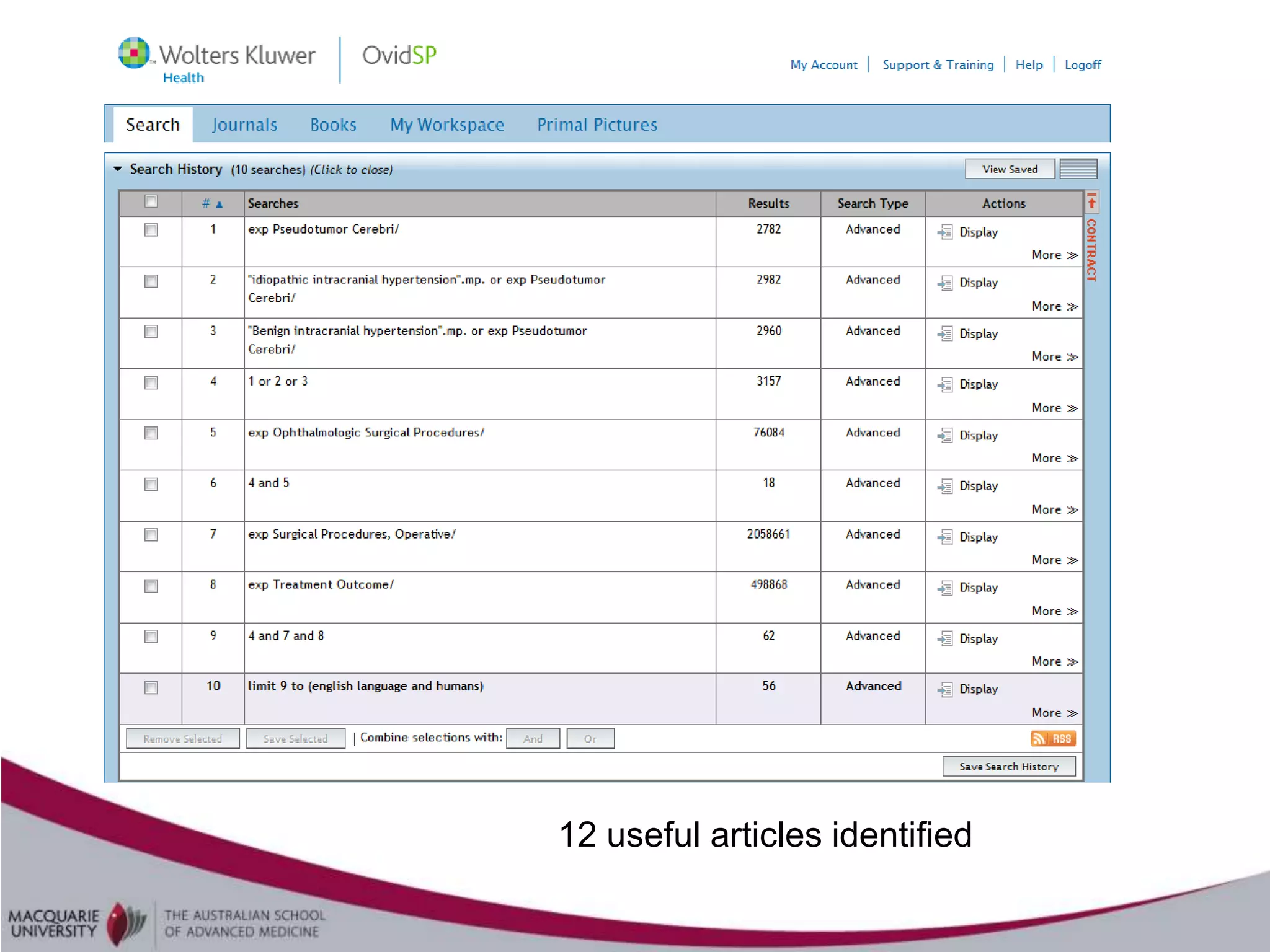
![Search strategy
• P = Idiopathic intracranial hypertension
• I = Optic nerve fenestration
• [C = Other surgical procedures (eg CSF shunting;
sinus stenting) ]
• O = Treatment outcomes
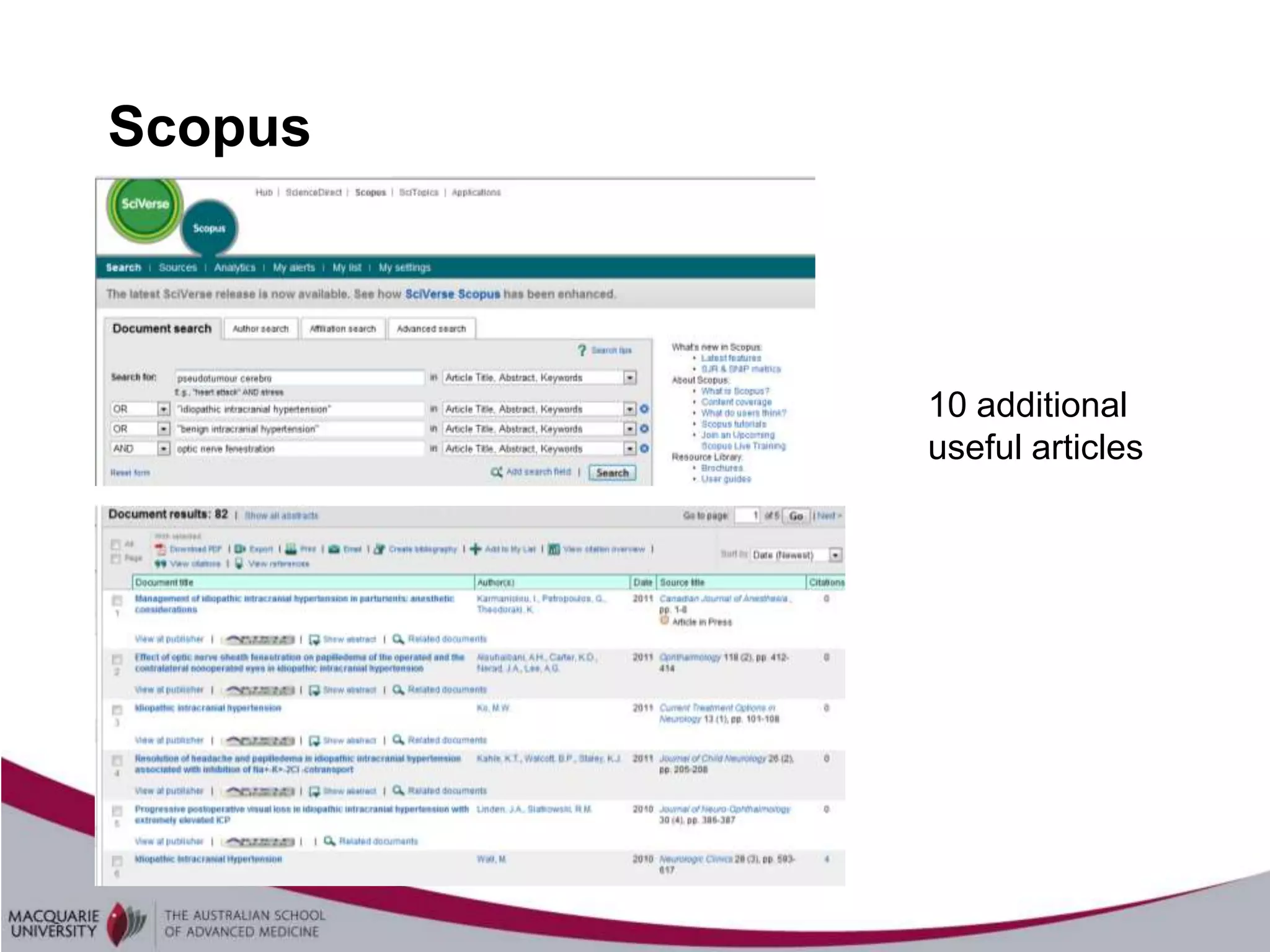
• Cochrane, Ovid Medline, Scopus, Google Scholar
• MeSH terms: “Pseudotumour cerebri” ; “ophthalmologic surgical
procedures”](https://image.slidesharecdn.com/idiopathicintracranialhypertension-120103174633-phpapp02/75/Idiopathic-intracranial-hypertension-4-2048.jpg)