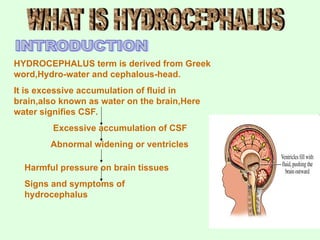
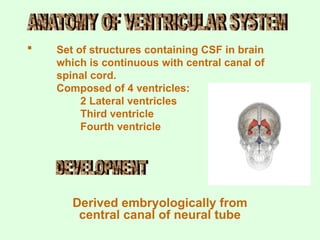
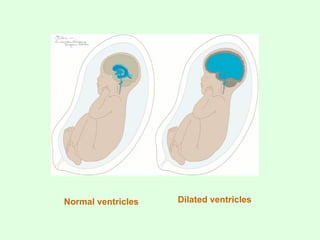
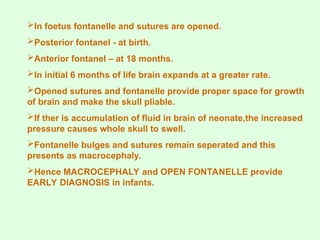
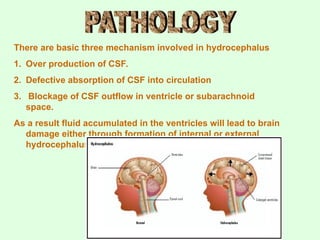
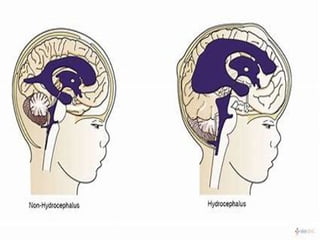
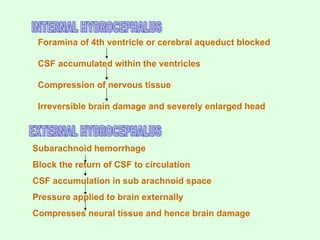
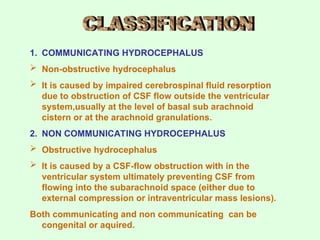
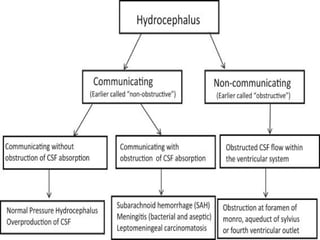
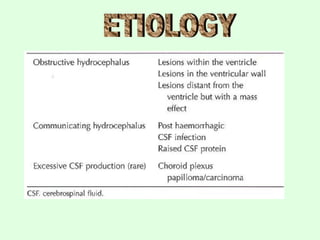
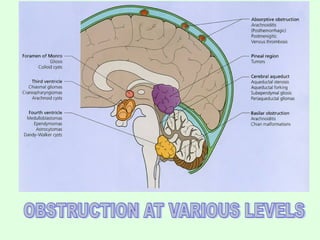
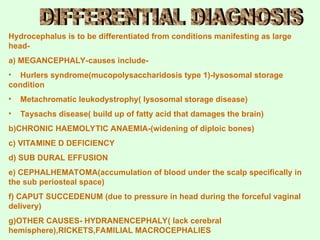
Hydrocephalus, derived from Greek meaning 'water on the brain,' is characterized by an excessive accumulation of cerebrospinal fluid (CSF) in the brain, leading to harmful pressure on brain tissues. It predominantly affects both children and adults, with an incidence of 1 in 500 live births, and can be caused by various factors, including congenital malformations and acquired conditions. Diagnosis is made through clinical evaluation and imaging techniques, and management typically involves surgical options like shunting to alleviate the increased intracranial pressure.




![Management of hydrocephalus depends on the underlying cause and
severity of symptoms
MEDICAL MANAGEMENT
This is a conservative approach for mild & slowly progressive
hydrocephalus or cases where surgery is not indicated
Acetazolamide[25 -100mg/kg/min]. - diuretic
Oral glycerol – diuretic
SURGICAL MANAGEMENT
It includes-
a)Removing of a causative mass leison
Intracranial mass lesion usually present with obstructive hydrocephalus
It includes tumor removal and decompression of CSF pathway using
EVD(External ventricular drainage) to cover early post operative period.
b) Ventricular shunting
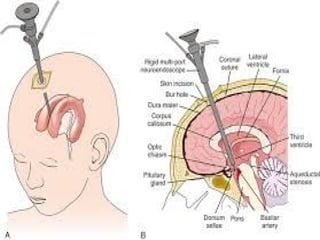
c) 3rd
ventriculostomy](https://image.slidesharecdn.com/hydrocephalus-241207160454-35e36669/85/Hydrocephalus-ppt-49-320.jpg)