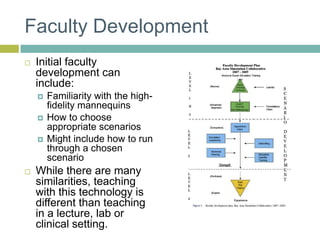
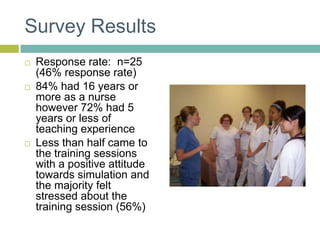
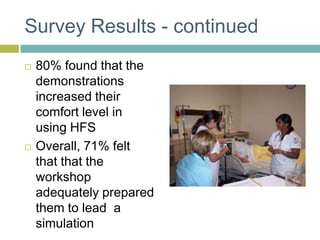
1) A workshop was developed to prepare clinical nursing faculty for using simulation in teaching. A survey found that while the workshop increased comfort, more preparation was still needed for faculty to lead simulations independently.
2) Implications included developing a DVD for additional support and making the workshop mandatory for new faculty. Ongoing development is also needed to address the disconnect between what students and faculty feel helps learning.
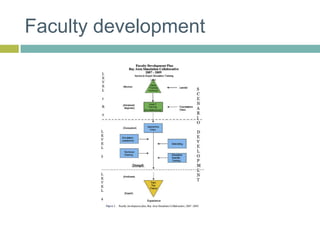
3) Future faculty development needs to go beyond basics and further prepare instructors to successfully facilitate simulation-based teaching.