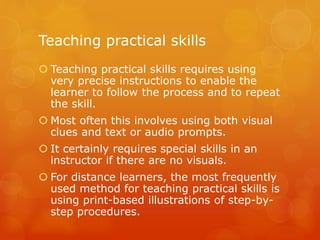
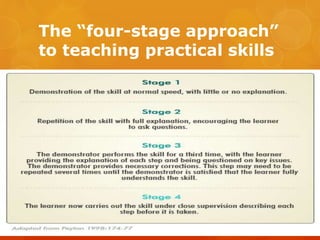
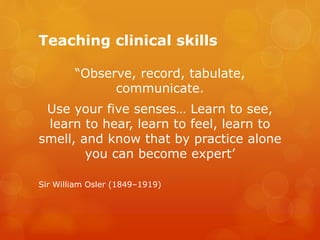
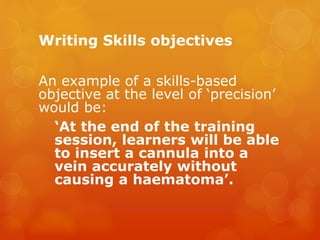
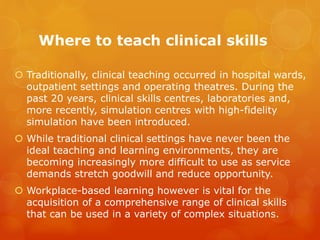
The document discusses teaching practical and clinical skills. It defines practical skills as those requiring physical dexterity and human intervention, while clinical skills refer to examinations and procedures around sick patients. It recommends teaching practical skills using precise visual and audio instructions. The four-stage approach to teaching involves demonstration, learner practice with feedback, independent practice, and competence assessment. Effective teaching of clinical skills requires using different environments like clinical settings, skills labs, and simulations while catering to diverse learner needs and styles.