Third-year nursing students at a university were surveyed about their learning styles and satisfaction with high-fidelity simulation (HFS). The majority of students were found to have a diverging learning style, which prefers reflecting on experiences. Students also scored highest on active experimentation, indicating a preference for learning through experiences rather than theoretically. Overall, students were highly satisfied with HFS and felt it incorporated effective teaching strategies and helped with clinical learning. However, further examination is needed to ensure HFS consistently helps prepare students for practice by accommodating different learning styles and characteristics.






![More simulations would be beneficial in applying our
understanding and prioritising patient needs.
dParticipant #27
There should be more simulations that aren’t neces-
sarily marked as an assessment but allows us more
opportunities to practice to different scenarios.
dParticipant # 60
Participants believed increasing the frequency of simu-
lations would better equip them to prioritize patient needs
and assist them to experience a diverse range of clinical
scenarios. Simulation design included comments on the
high ratio of participant to manikin (4:1) and its negative
impact on the simulation experience.
I believe that 4 student participants is too much, and
can hinder other students learning experience in the
simulation.
dParticipant # 2.
The challenges in treating a manikin like a real person
rather than using student volunteers as the patient to
improve the fidelity of the simulation and the negative
impact of the reduced length of debrief on learning were
also hindrances to learning.
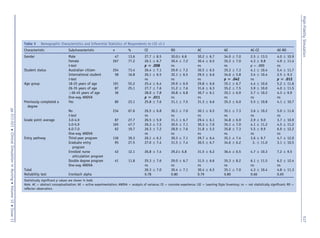
The response rate for the Reflective Thinking and Simu-
lation survey was 346; however, n ¼ 32 (9.3%) participant
questionnaires were excluded from the study due to incom-
plete or incorrect responses, resulting in analysis of 314
participant Kolb LSI v 3.1 surveys. Most participants who
responded to the LSI v 3.1 were female n ¼ 267 (77.2%) and
between the ages of 18 and 25 years (n ¼ 191, 55.2%). Almost
74% of respondents were domestic students (Australian
citizens) (Table 5). Sixty-seven percent of participants had
not previously completed a degree and just under half
(47.7%) of the participants had a GPA ranging from 5.0 to 5.9.
LSI: Learning Characteristics
The mean concrete experience [CE] total score was lower
(26.3) than the other three learning characteristics (reflector
observation [RO] ¼ 30.4; abstract conceptualization
[AC] ¼ 30.4; and active experimentation [AE] ¼ 35.1).
When compared to the Kolb LSI v3.1 total normative group
(Kolb Kolb, 2005), the results of this study are similar,
with small differences in RO (30.4/28.2) and AC (30.4/
32.2). The mean CE score was significantly greater in
male students compared to female students (Table 5). The
mean AE score was greater in Australian citizen/domestic
students compared to international students. The mean
score for CE was significantly greater in the 36- to 45-
year-old age group, compared to the 18- to 25-year-old
age category (p ¼ .027). The analysis of the mean AE score
revealed no significant differences for participants who had
completed a previous degree, GPA between 6.0 and 7.0 and
whose entry pathway was via enrolled nurse articulation.
The overall mean score for the AE-RO scale was 4.8 and
4.3 for the AC-CE scale. Internal consistency was good
(0.80) for the CE total score. Cronbach’s alpha improved to
0.81 if item 11.1 was removed. The RO subscale demon-
strated a good internal consistency with a Cronbach’s alpha
of 0.8. An increase in this value to 0.81 was achieved with
the removal of item 5.2. Both AC and AE displayed good
internal consistency, with Cronbach alphas of 0.79 and 0.80,
respectively. An increase in Cronbach’s alpha for AE
resulted with the removal of item 3 (0.80). These values
are similar to those previously reported by Kolb and Kolb
(2005) in the norm subsample of online LSI users
(n ¼ 5,023). Reliability of AC-CE and AE-RO subscales
were 0.66 and 0.65, respectively. Removal of items 5C
from the AC-CE subscale and item 5B from the AE-RO sub-
scale resulted in an increase in the Cronbach’s alpha values
to 0.68 and 0.67, respectively.
LSI: Learning Styles
The learning styles of the third-year undergraduate nursing
students were diverging (n ¼ 103; 29.8%), followed by
accommodating (n ¼ 87; 25.1%), then assimilating
(n ¼ 67; 19.4%), closely followed by converging
(n ¼ 57; 16.5%). A chi-square test for independence
indicated no significant association between gender and
learning styles and age and learning styles (Table 6).
Discussion
The subscale AE was the highest mean score compared to
CE as the lowest mean score. This suggests that simulation is
a good fit for third-year undergraduate nursing students.
Students with this type of preferred learning characteristic
have learning skills for success in technology careers such as
nursing and medicine (Shinnick Woo, 2013). It identified
that these students have the ability to learn from primarily
Table 6 Chi-Square Analysis of Learning Styles for Gender and Age (n ¼ 314)
Demographics Accommodating Diverging Converging Assimilating
Gender c2
(1) ¼ 0.03, p ¼ .866 c2
(1) ¼ 0.10, p ¼ .757 c2
(1) ¼ 1.55, p ¼ .213 c2
(1) ¼ 1.80, p ¼ .180
Age c2
(2) ¼ 0.32, p ¼ .854 c2
(2) ¼ 4.62, p ¼ .099 c2
(2) ¼ 1.70, p ¼ .427 c2
(2) ¼ 0.40, p ¼ .818
High-Fidelity Simulation 518
pp 511-521 Clinical Simulation in Nursing Volume 12 Issue 11](https://image.slidesharecdn.com/8a964021-45a9-455c-8da1-093e61ed0e78-160921064642/85/High-fidelity-simulation_Descriptive-analysis-of-student-learning-styles_CSN-8-320.jpg)


![http://dx.doi.org/10.1016/j.nedt.2012.04.004. Retrieved from http://
www.sciencedirect.com/science/article/pii/S0260691712001098.
Smith E. (2011). Teaching critical reflection. Teaching in higher educa-
tion [serial online]. Ipswich, MA: Academic Search Elite;16(2):
211-223.
Swanson, E. A., Nicholson, A. C., Boese, T. A., Cram, E., Stineman, A. M.,
Tew, K. (2011). Comparison of selected teaching strategies incorporating
simulation and student outcomes. Clinical Simulation in Nursing, 7(3),
e81-e90, ISSN 1876-1399. http://dx.doi.org/10.1016/j.ecns.2009.12.011.
Teixeira, C. R. d. S., Kusumota, L., Pereira, M. C. A., Braga, F. T. M. M.,
Gaioso, V. P., Zamarioli, C. M., de Carvalho, E. C. (2014). Anxiety
and performance of nursing students in regard to assessment via clinical
simulations in the classroom versus filmed assessments. Investigacion
y Educacion En Enfermerıa, 32(2), 270-279, Retrieved from http://
search.proquest.com/docview/1552719984?accountid¼13380.
Tutticci, N., Lewis, P. A., Coyer, F. (2016). Measuring third year under-
graduate nursing students’ reflective thinking skills and critical reflec-
tion self-efficacy following high fidelity simulation: A pilot study.
Nurse Education in Practice, 18(5), 52-59.
Vygotsky, L. (1978). Interaction between learning and development.
In: Vygotsky, L. (Ed.), Mind and Society. Cambridge, MA: Har-
vard University Press. (pp. 79-91).
Wotton, K., Davis, J., Button, D., Kelton, M. (2010). Third-year under-
graduate nursing students’ perceptions of high-fidelity simulation. Jour-
nal of Nursing Education, 49(11), 632-639. http://dx.doi.org/10.3928/
01484834-20100831-01.
High-Fidelity Simulation 521
pp 511-521 Clinical Simulation in Nursing Volume 12 Issue 11](https://image.slidesharecdn.com/8a964021-45a9-455c-8da1-093e61ed0e78-160921064642/85/High-fidelity-simulation_Descriptive-analysis-of-student-learning-styles_CSN-11-320.jpg)