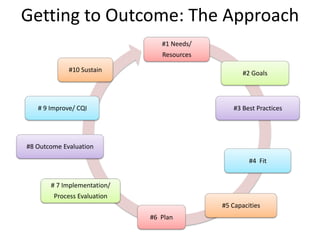
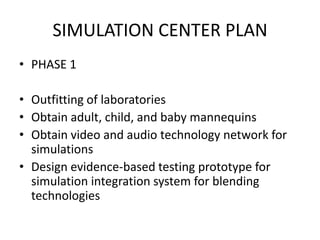
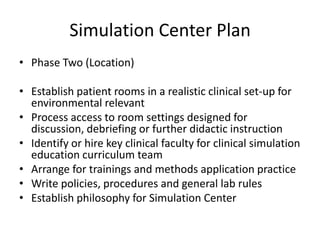
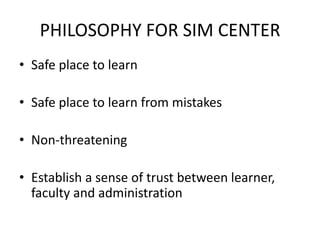
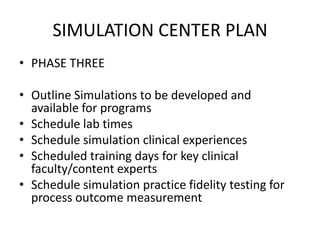
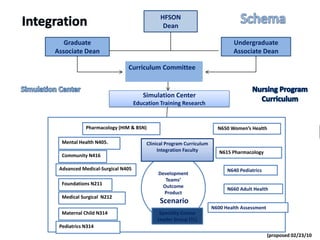
1. The document discusses setting up a simulation center infrastructure using an evidence-based approach to assess outcomes. It outlines steps such as developing a vision, strategic planning, and appraising resources and barriers.
2. Research results show that simulations combined with lecture can increase nursing students' self-confidence and satisfaction with their learning. Studies found simulations improved cognitive skills and the ability to answer test questions.
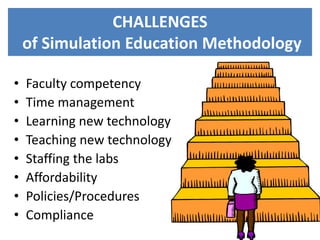
3. Challenges in simulation education include ensuring faculty competency, managing time and learning new technologies, and issues of affordability, policies, and staffing labs.