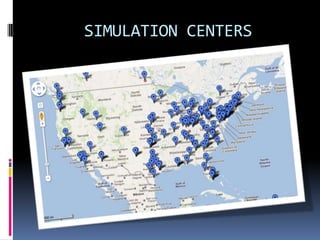
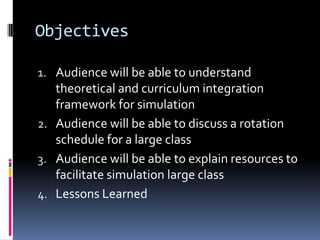
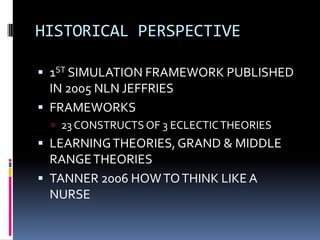
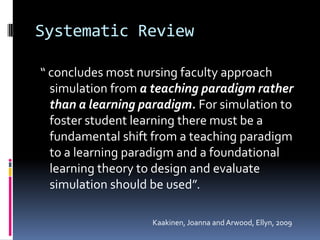
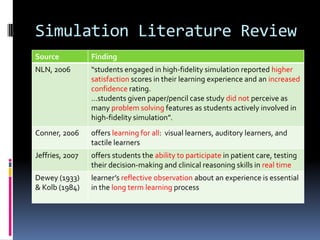
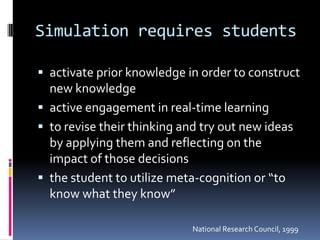
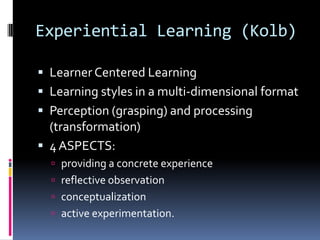
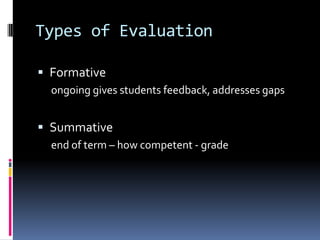
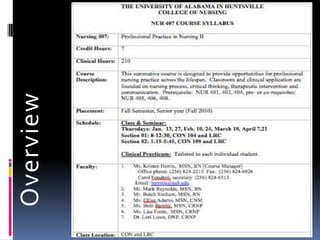
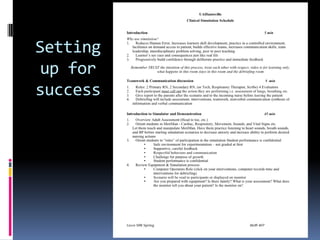
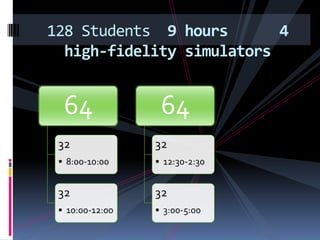
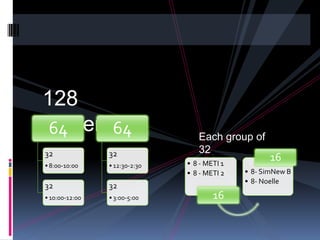
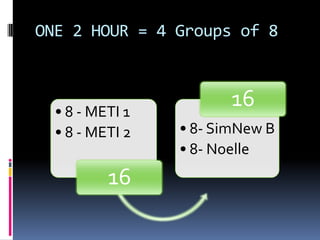
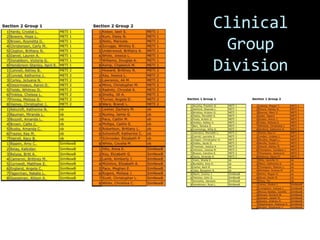
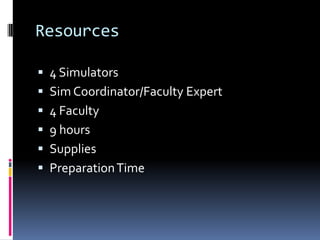
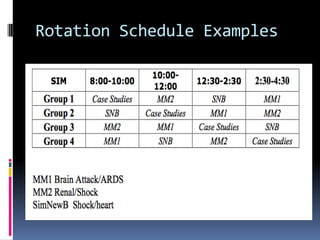
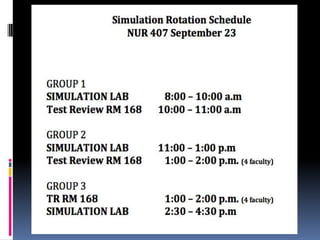
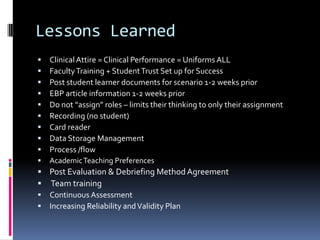
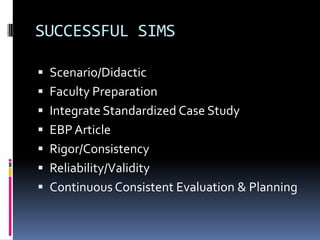
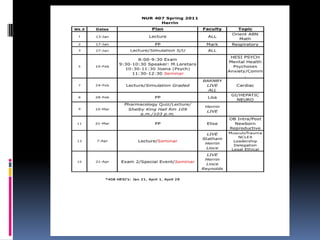
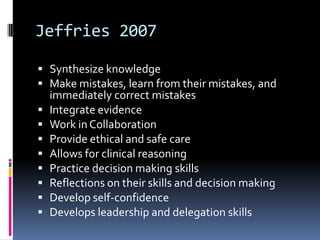
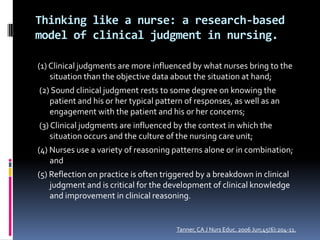
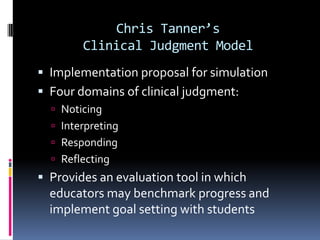
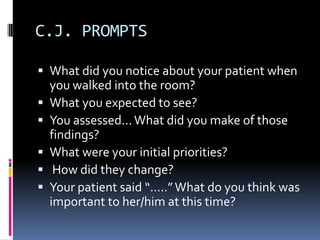
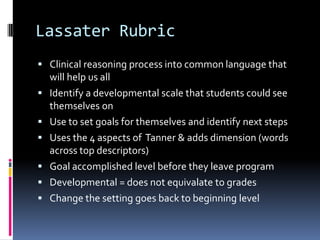
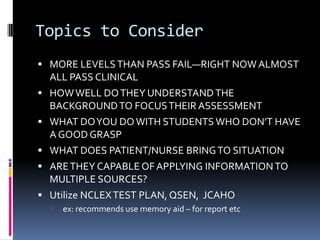
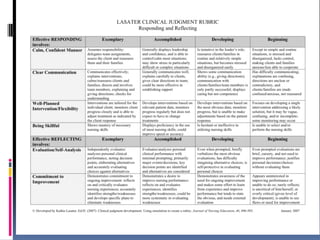
This document outlines a framework for integrating simulation in nursing education, emphasizing a shift from a teaching to a learning paradigm to enhance student engagement and clinical reasoning. It provides insights on the scheduling and resources needed for large class simulations, along with lessons learned for improving the effectiveness of such educational experiences. Key references and theoretical models are presented to support the application of simulation as a teaching strategy in a nursing curriculum.