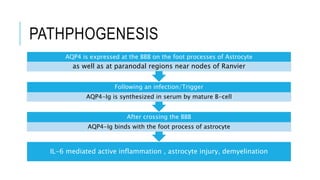
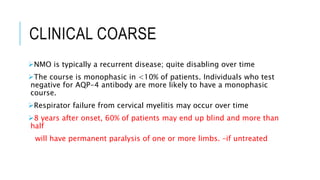
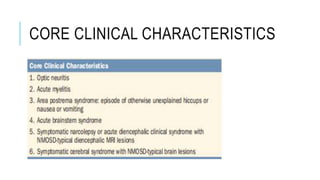
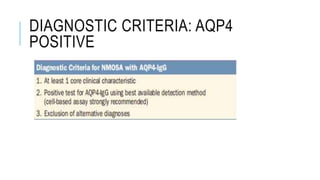
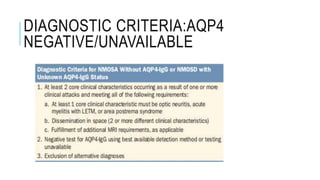
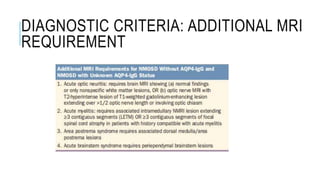
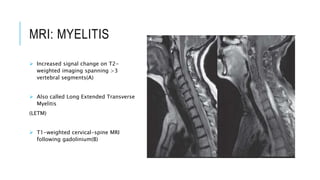
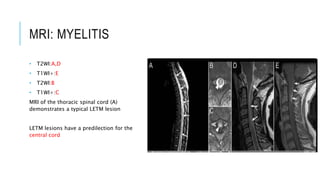
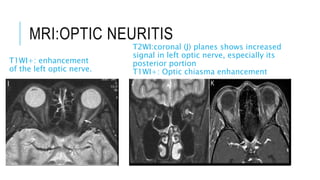
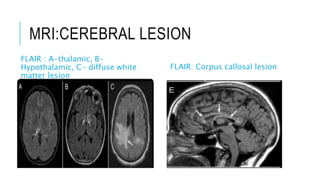
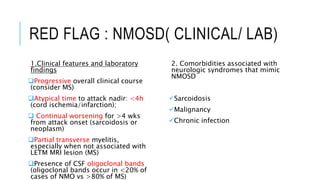
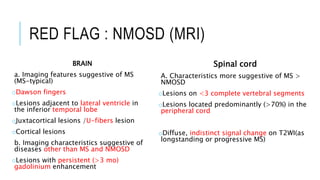
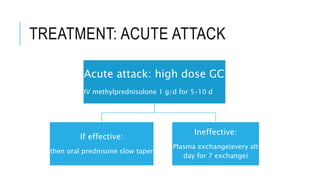
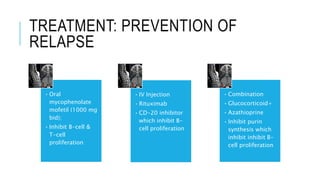
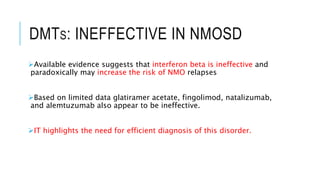
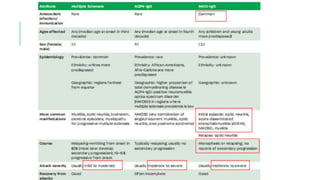
Neuromyelitis optica (NMO), also known as Devic's disease, is an inflammatory disorder characterized by demyelination of the optic nerve and spinal cord. It is associated with antibodies against aquaporin-4 (AQP4-IgG). The disease predominantly affects women and typically presents with episodes of optic neuritis and transverse myelitis. MRI often shows long extensive lesions of the spinal cord. Treatment involves high-dose steroids for acute attacks and immunosuppressants like mycophenolate mofetil or rituximab to prevent relapses. Distinguishing NMO from multiple sclerosis is important for treatment, as some therapies effective for MS may worsen NMO.