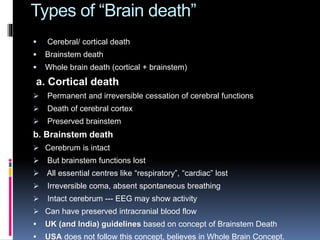
The document discusses brain death as a clinical syndrome characterized by irreversible loss of brain function while circulation may still persist. It outlines the definitions, criteria for diagnosing brain death, relevant guidelines, and legal aspects pertaining to organ donation in the context of brain death in India. The document also delves into the neurological examination process, including the apnea test, and acknowledges the differences between Indian and U.S. definitions of brain death.