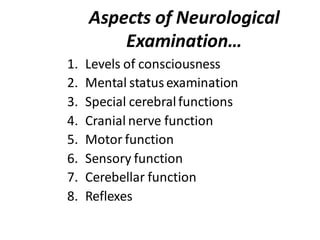
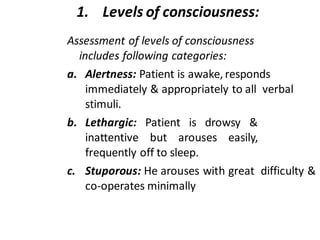
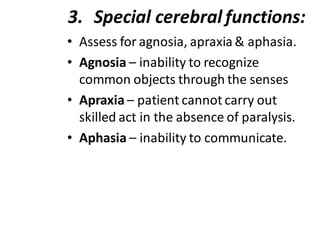
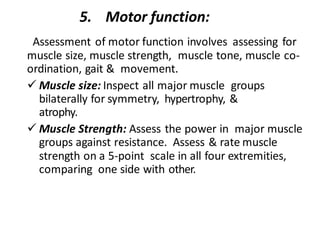
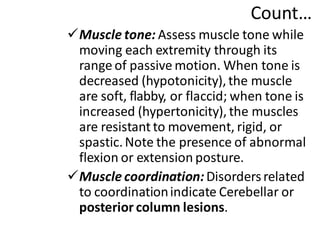
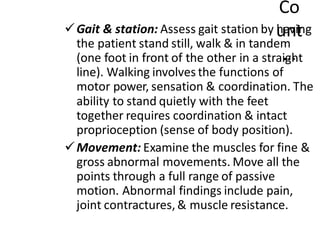
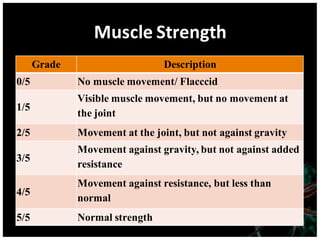
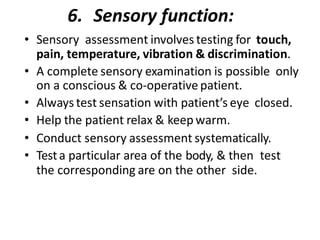
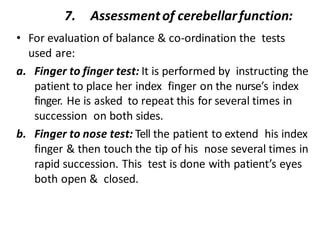
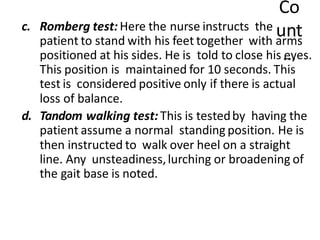
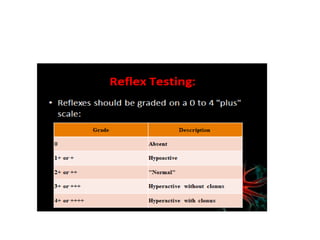
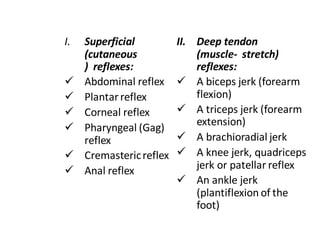
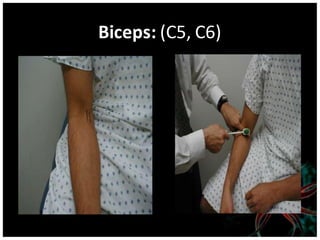
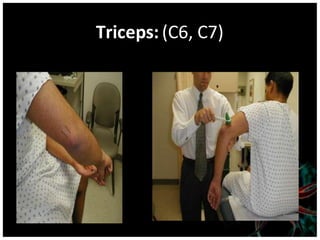
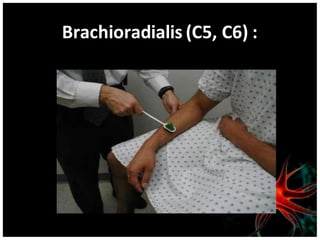
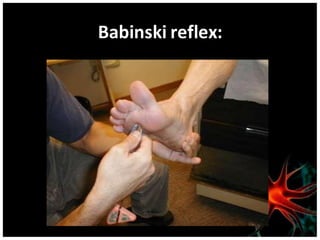
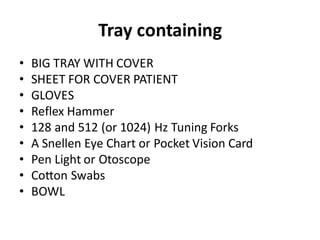
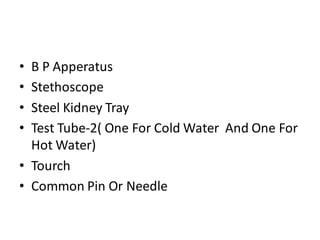
1. The neurological examination document outlines the process and components of examining a patient's nervous system, including terminology, indications, and aspects of the exam such as level of consciousness, cranial nerve function, motor function, and reflexes.
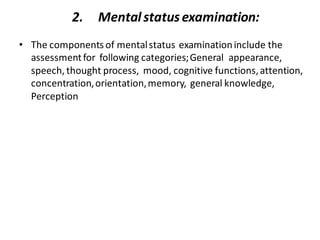
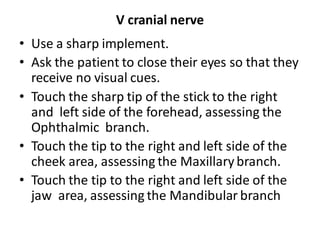
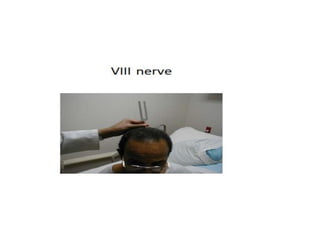
2. Nurses play an important role in conducting and documenting the neurological exam. This includes setting up equipment, assessing vital signs, performing tests of mental status, cranial nerves, motor skills, sensation, and reflexes, and communicating findings to doctors.
3. The goal of the neurological exam is to determine if there is any disease or abnormality present in the nervous system by thoroughly assessing multiple domains of neurological function.