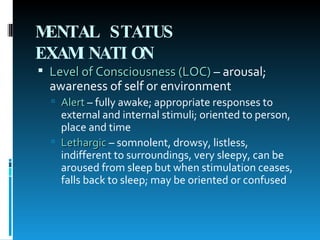
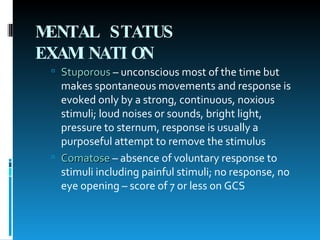
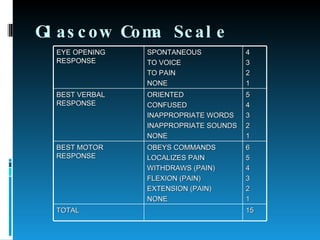
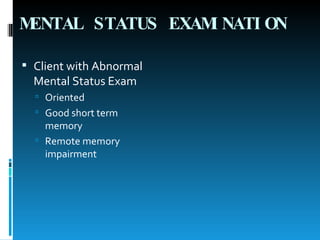
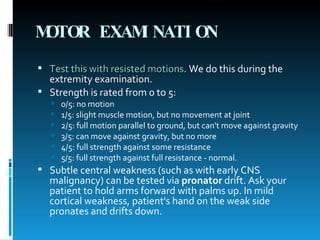
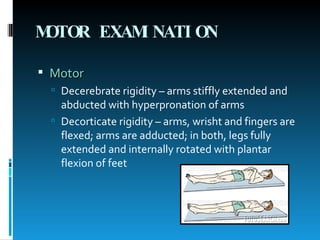
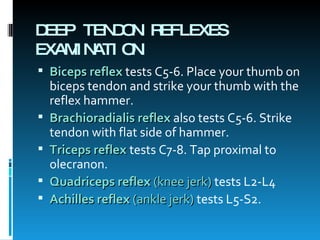
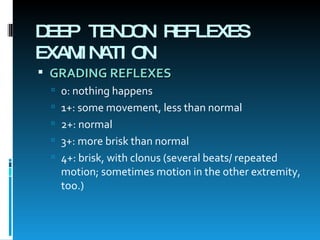
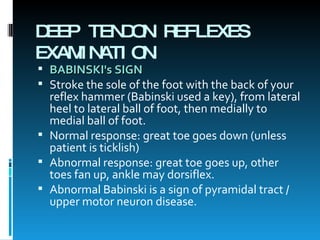
The document provides an overview of performing a neurologic exam, including testing of the cranial nerves, sensation, strength, reflexes, and coordination. It describes how to test each component and common abnormalities that may be observed, with the goal of being able to recognize neurologic deficits.