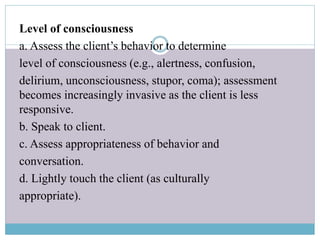
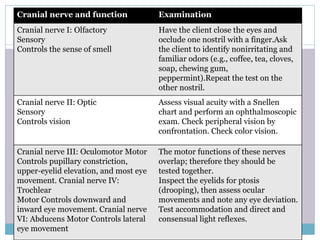
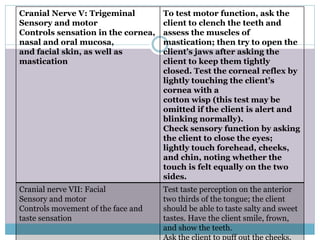
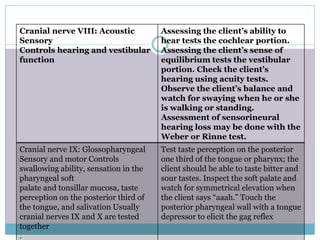
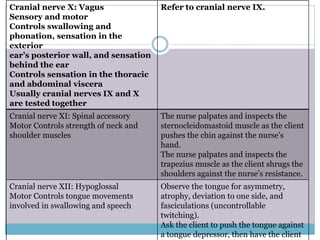
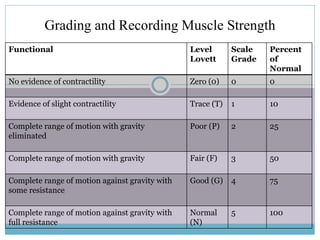
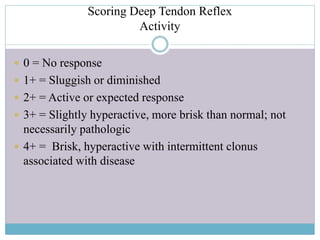
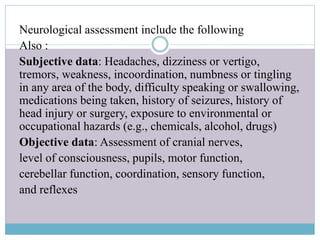
A neurological examination assesses the nervous system by testing sensory and motor responses, especially reflexes. It involves testing several areas including mental status, cranial nerves, muscle strength, gait, coordination, sensory function, and reflexes. Cranial nerve exams identify problems with the 12 cranial nerves by physical examination. A full neurological exam includes subjective and objective assessments as well as vital sign checks.