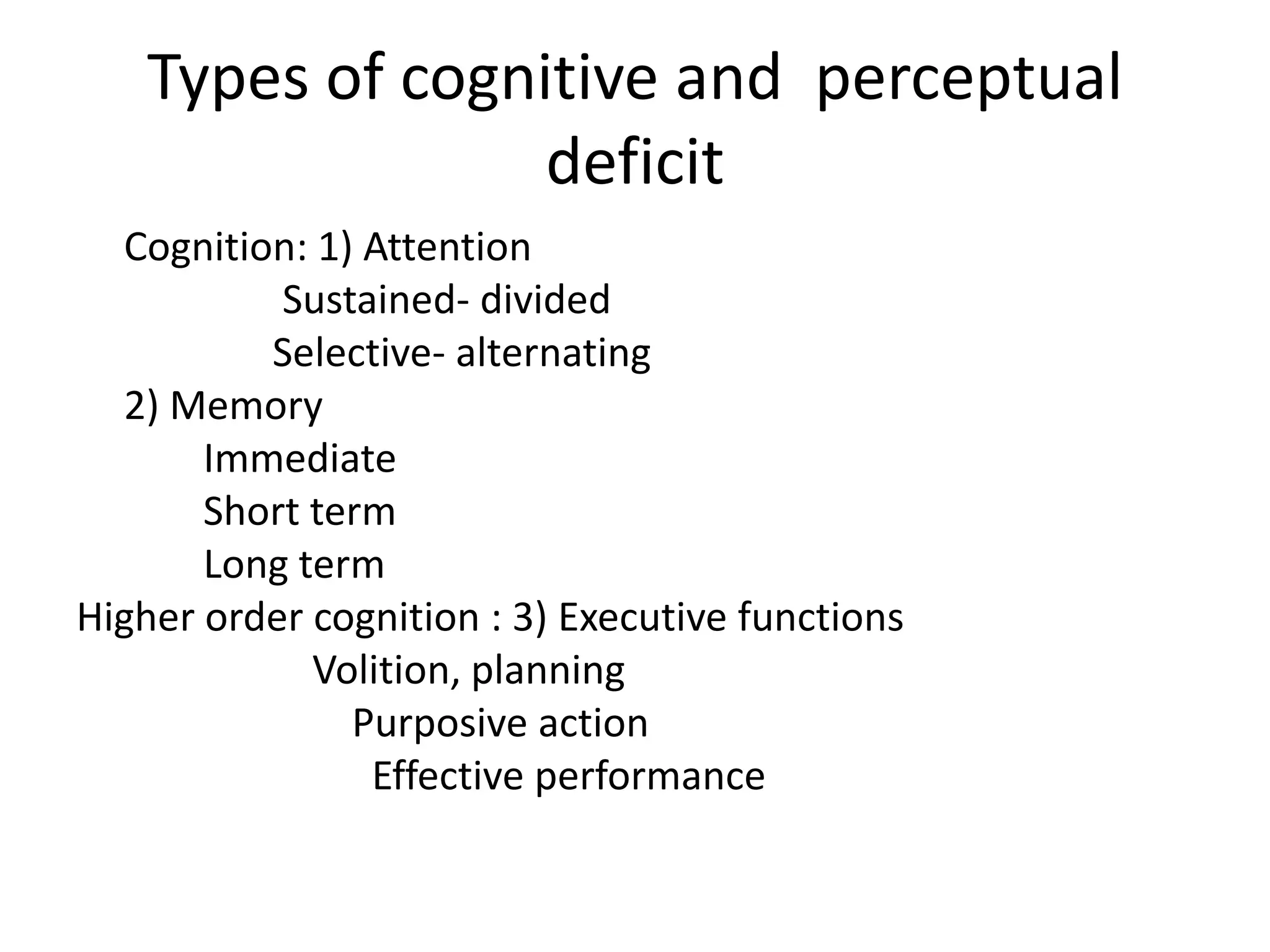
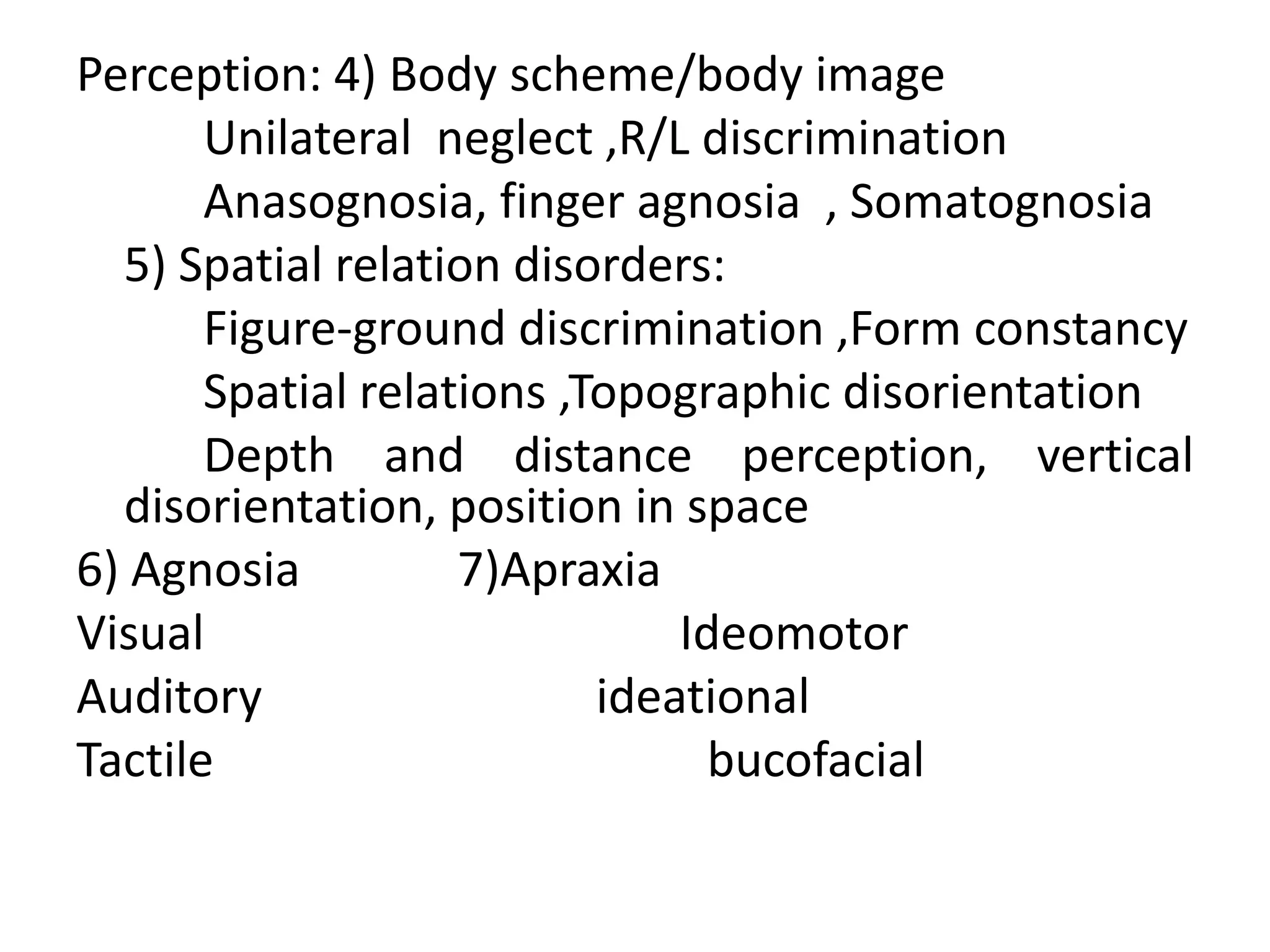
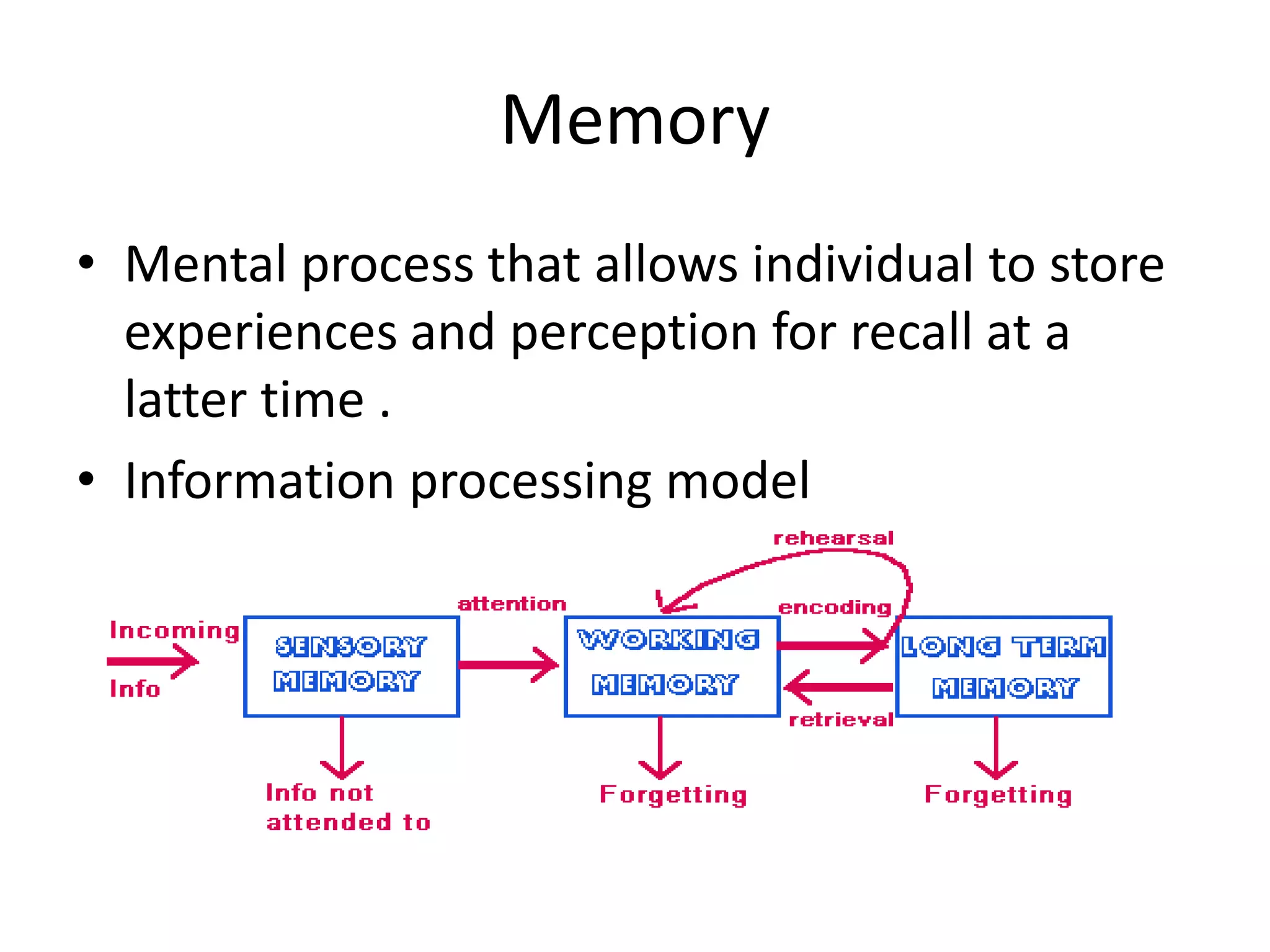
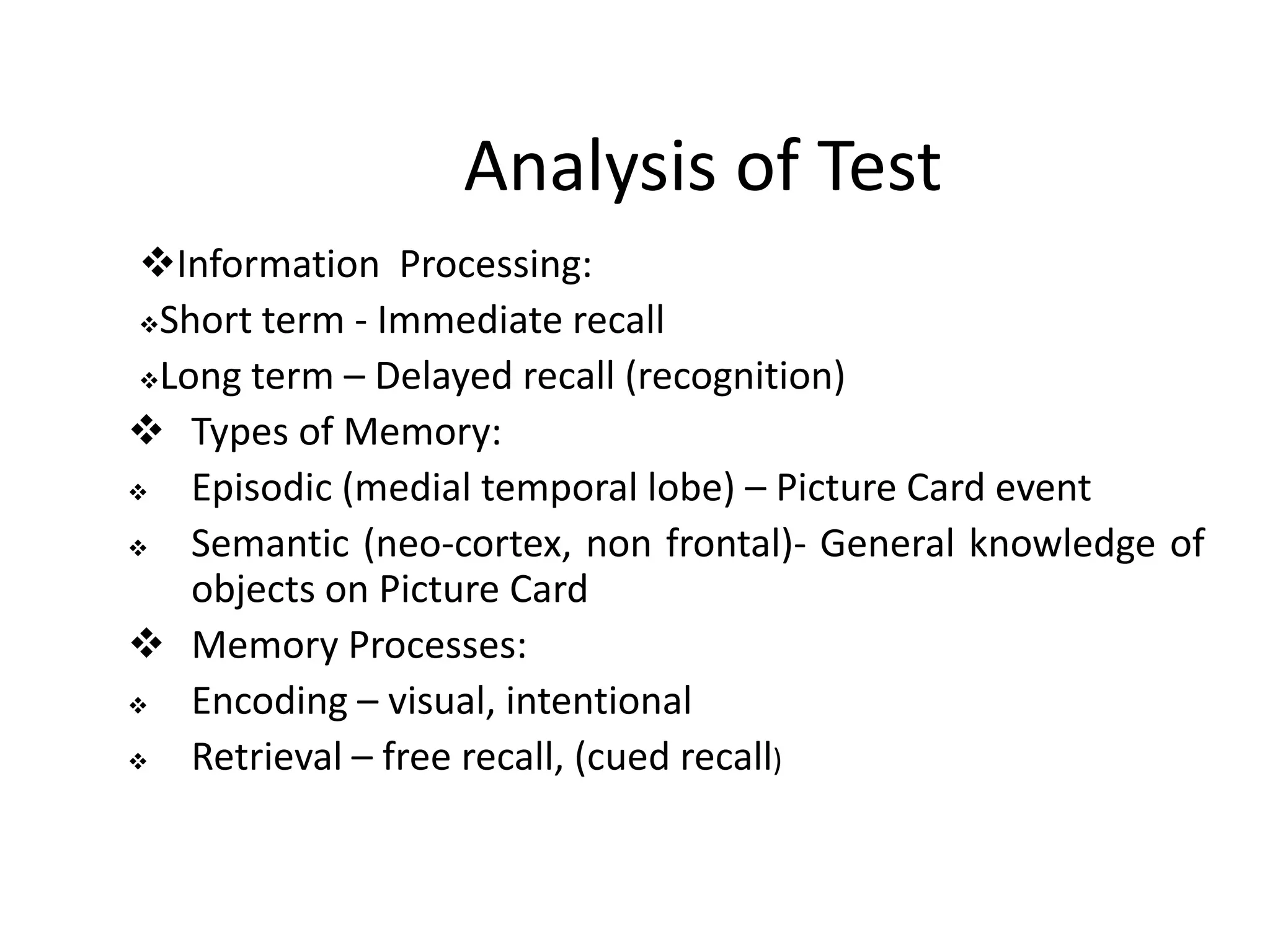
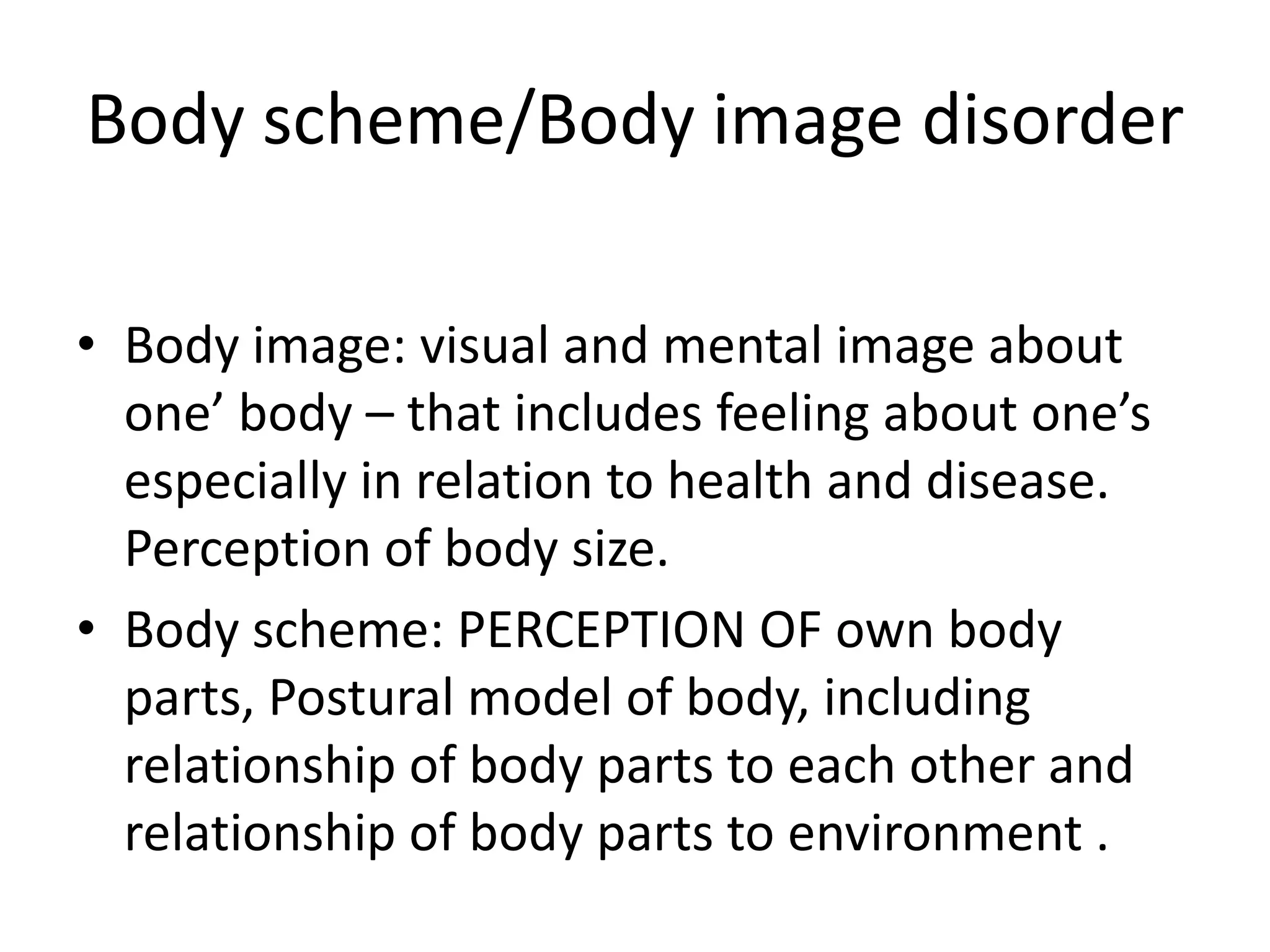
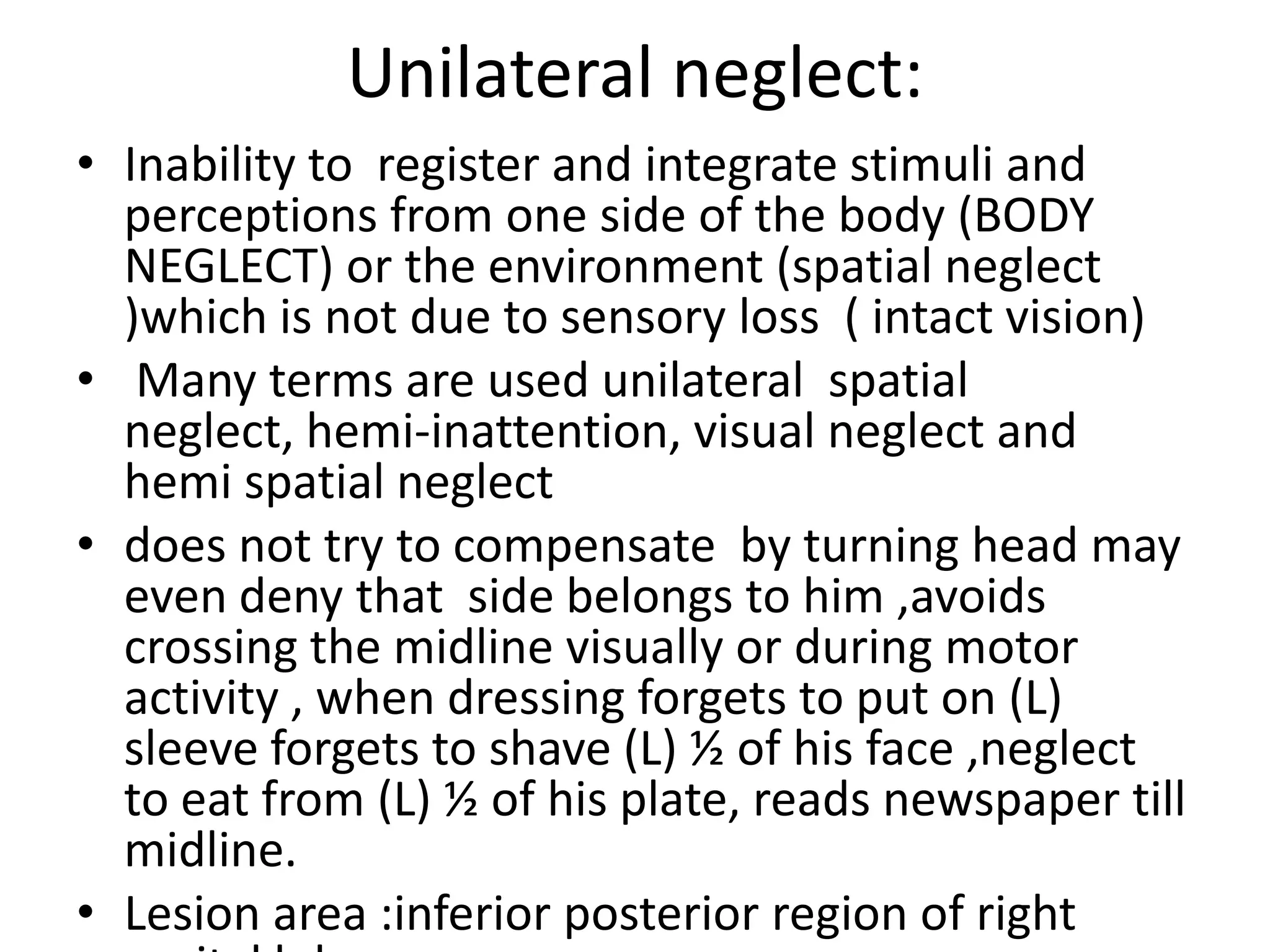
This document discusses perceptual and cognitive dysfunction. It begins by defining perception as the process of integrating sensory stimuli into meaningful information. Cognition is defined as the act of knowing, including awareness, reasoning, judgment, intuition and memory.
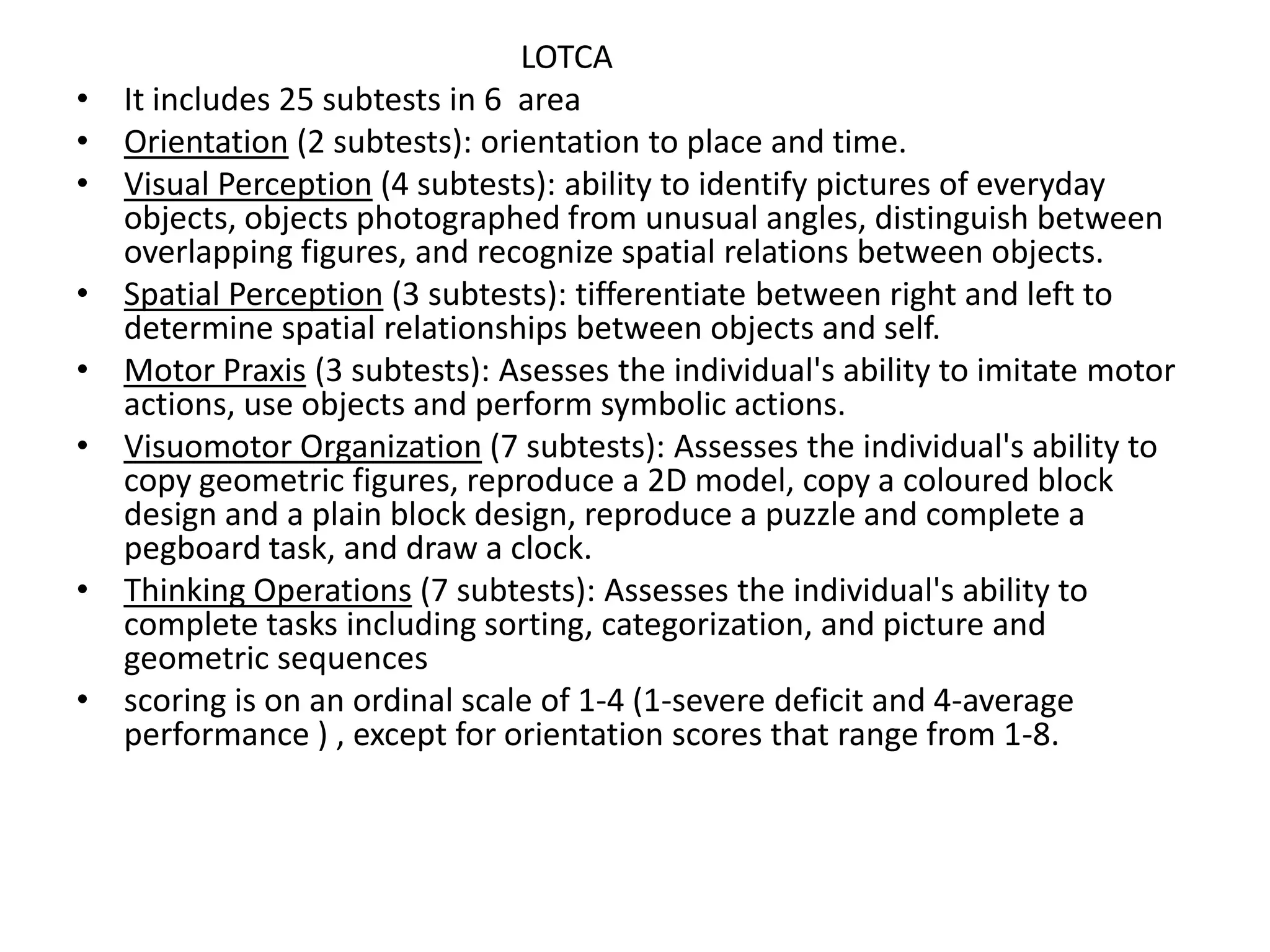
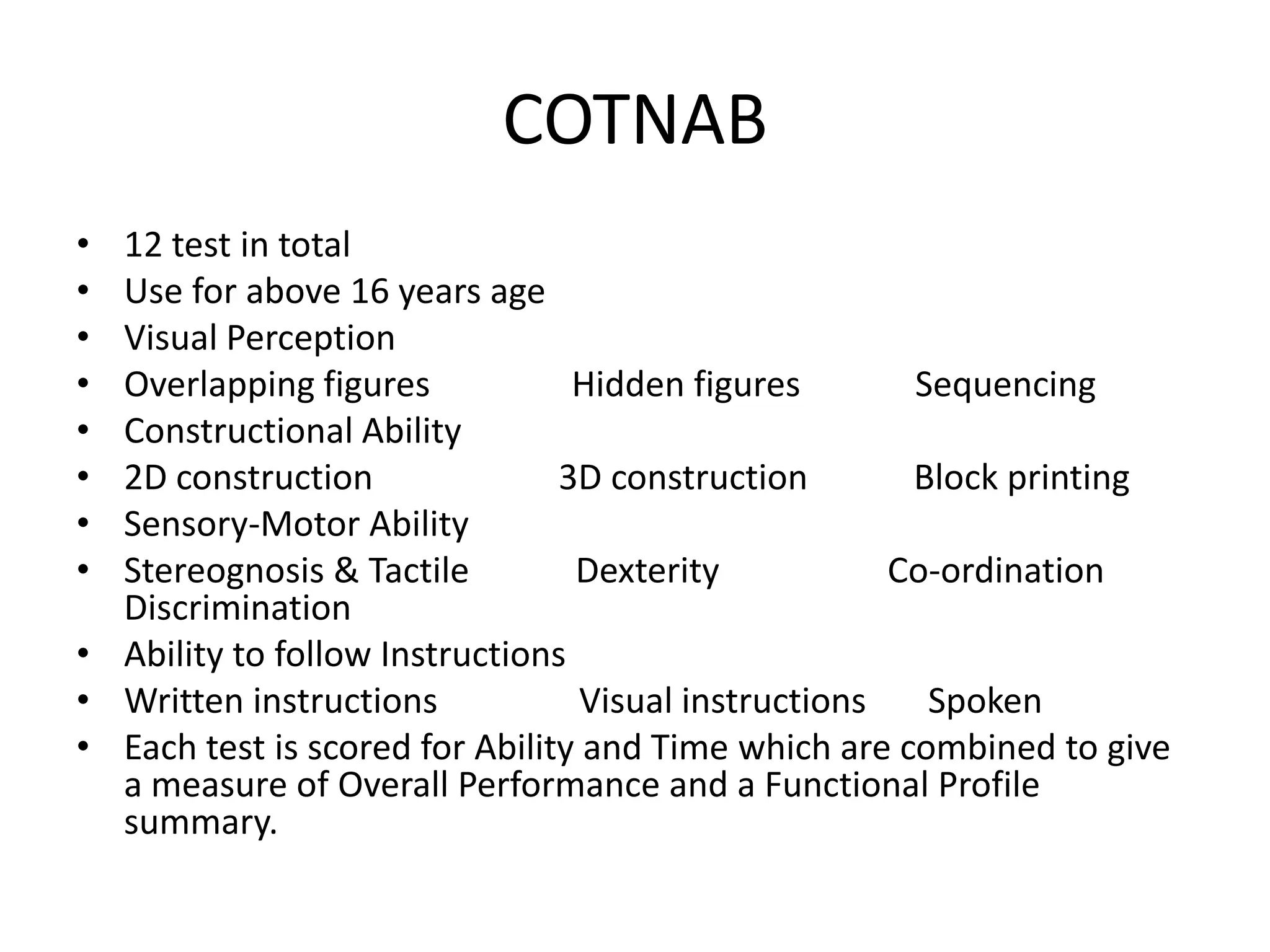
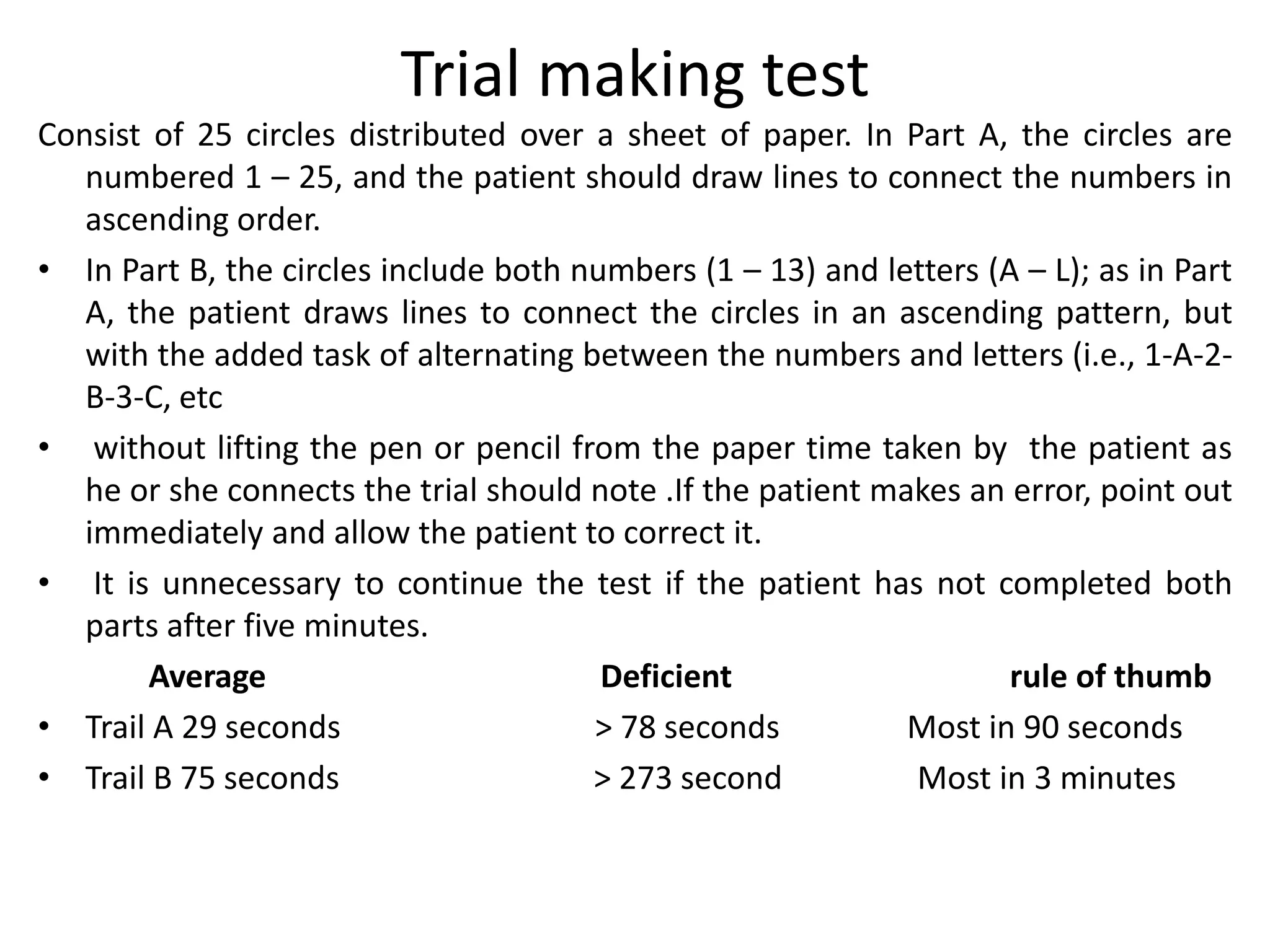
The document then discusses assessment of perceptual and cognitive deficits. It notes that perception is positively correlated with ability to perform activities of daily living and is a prerequisite for learning and rehabilitation. Clinical indicators of perception deficits include functional loss unexplained by motor or sensory deficits and deficient comprehension. Assessment aims to determine intact and affected perceptual abilities and how task performance is affected by deficits.
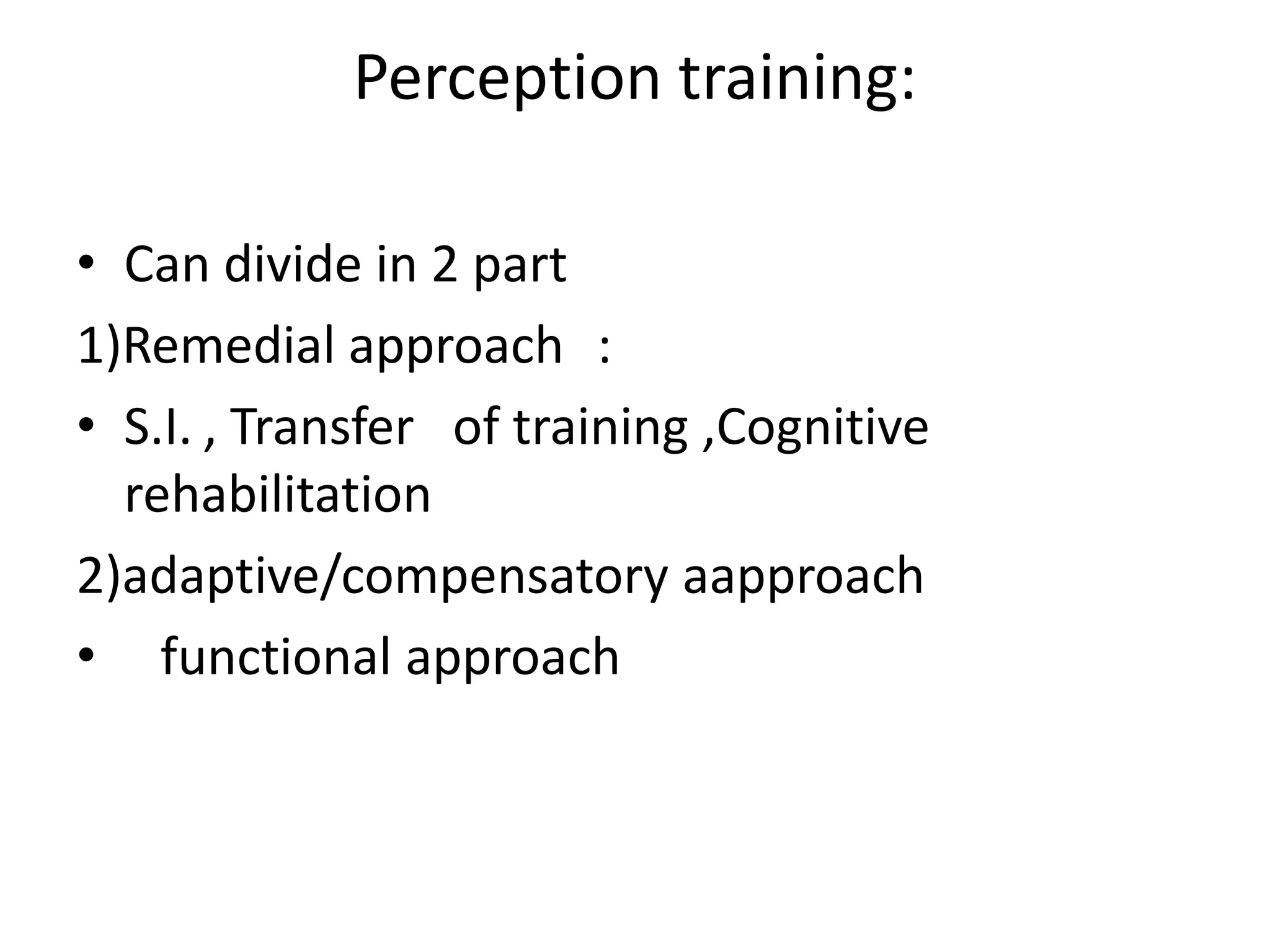
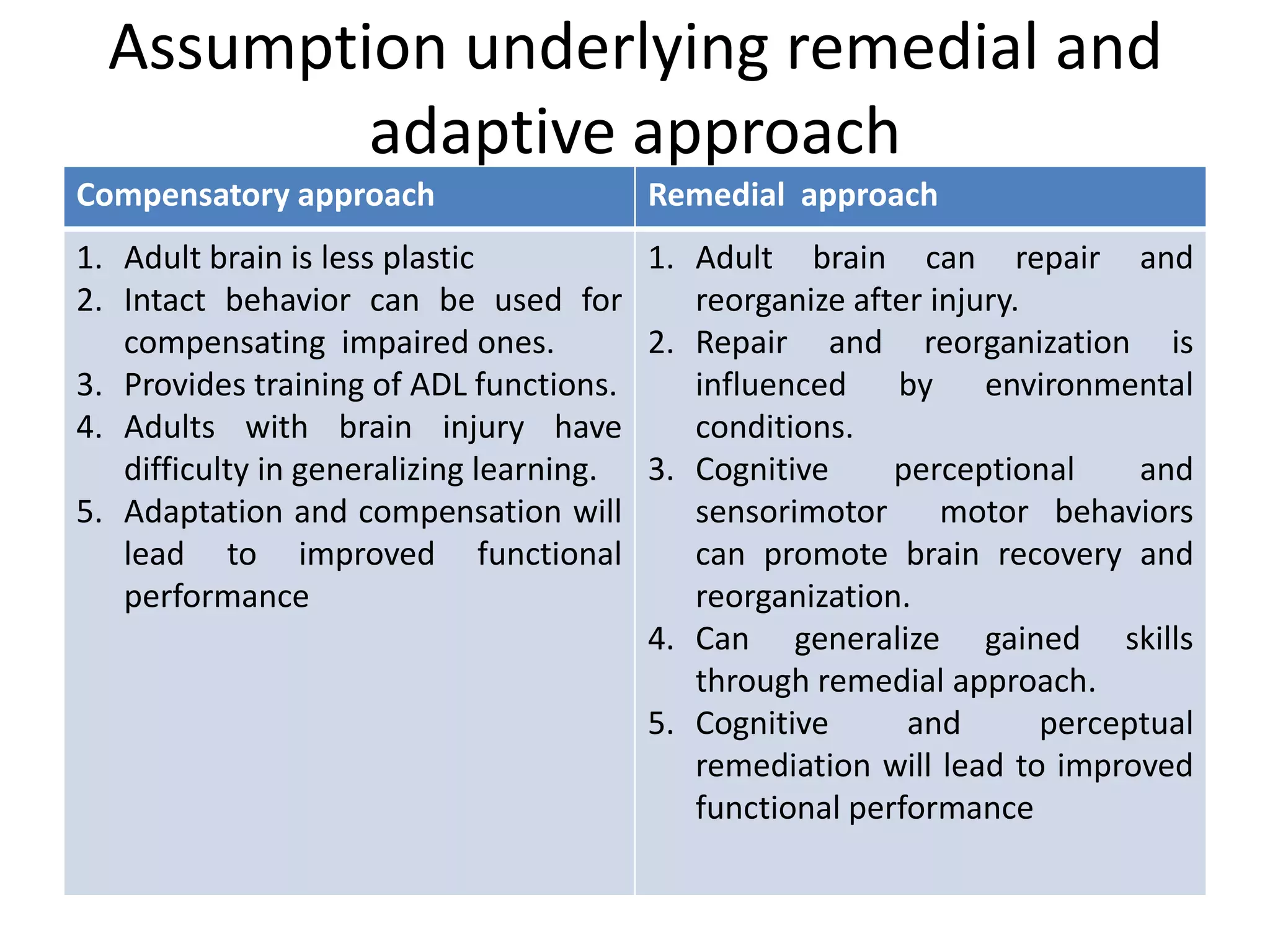
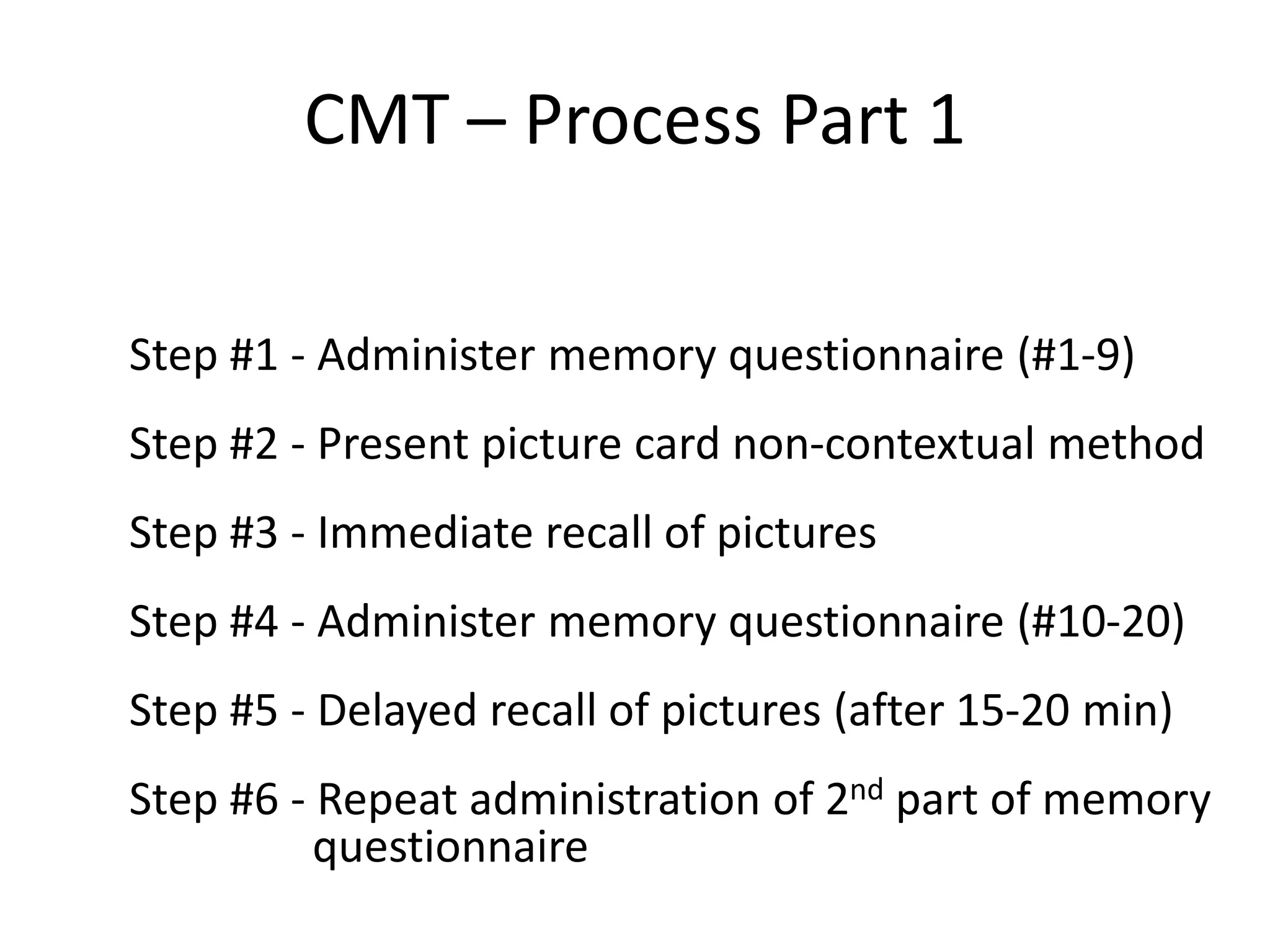
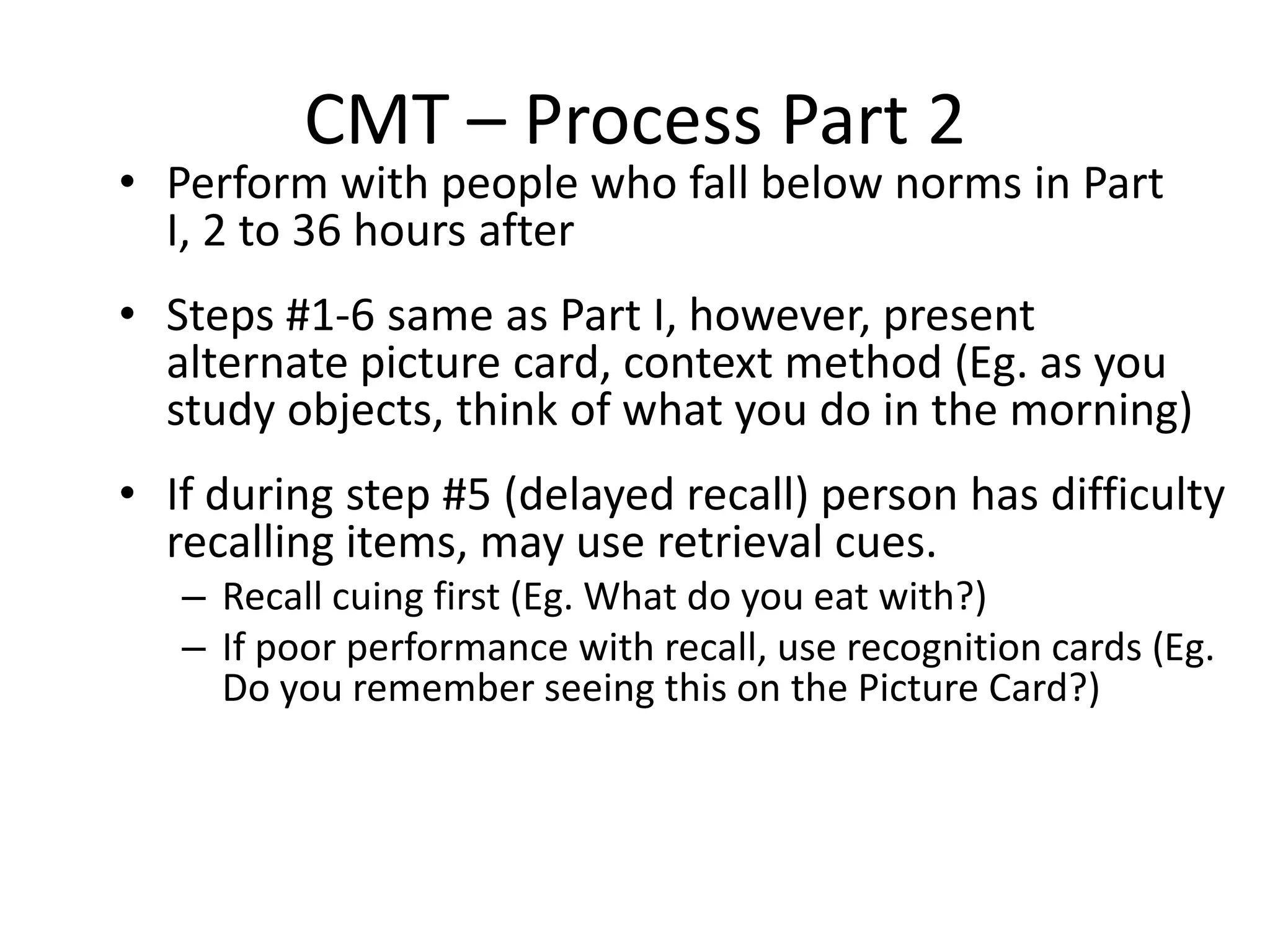
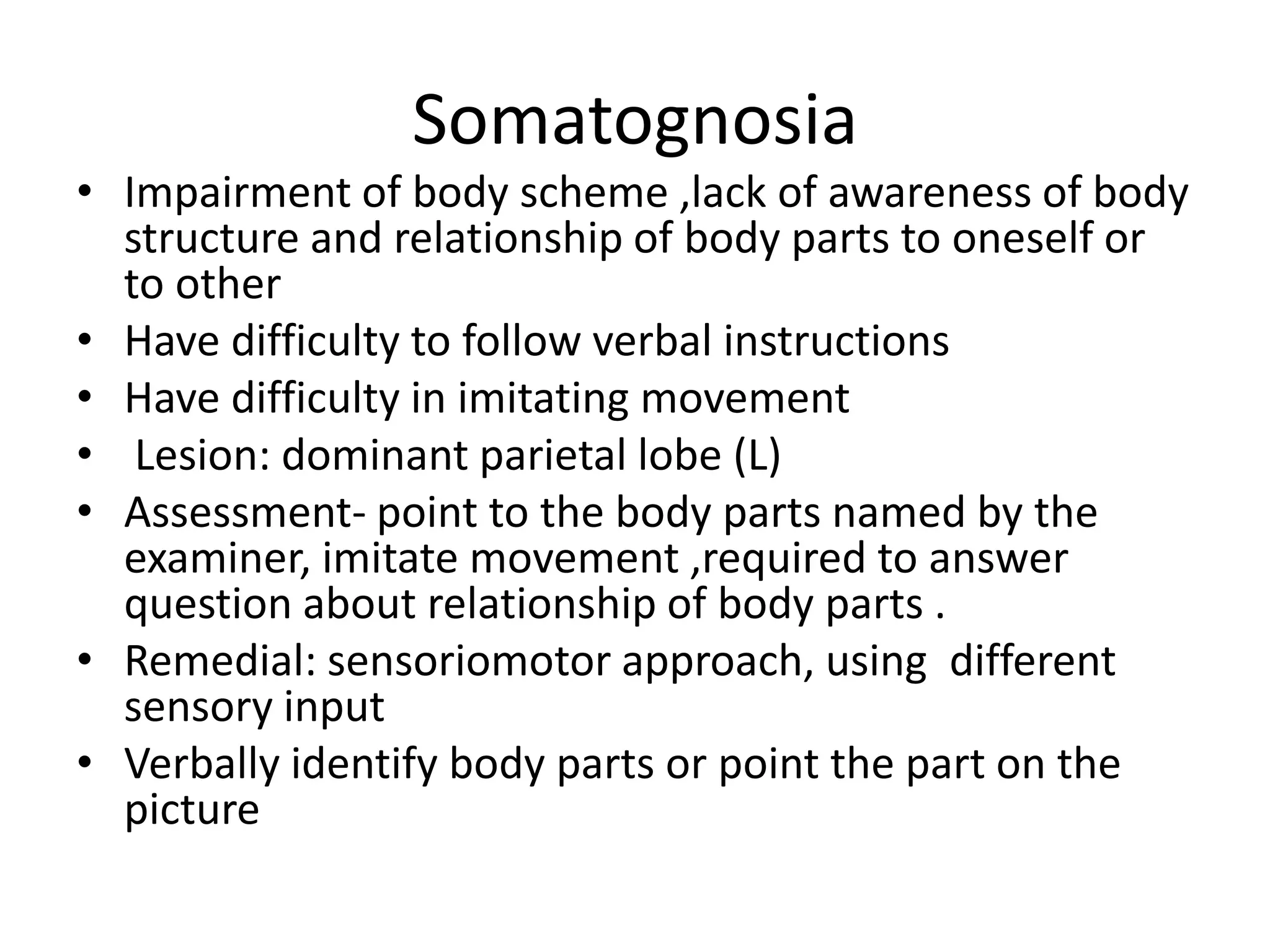
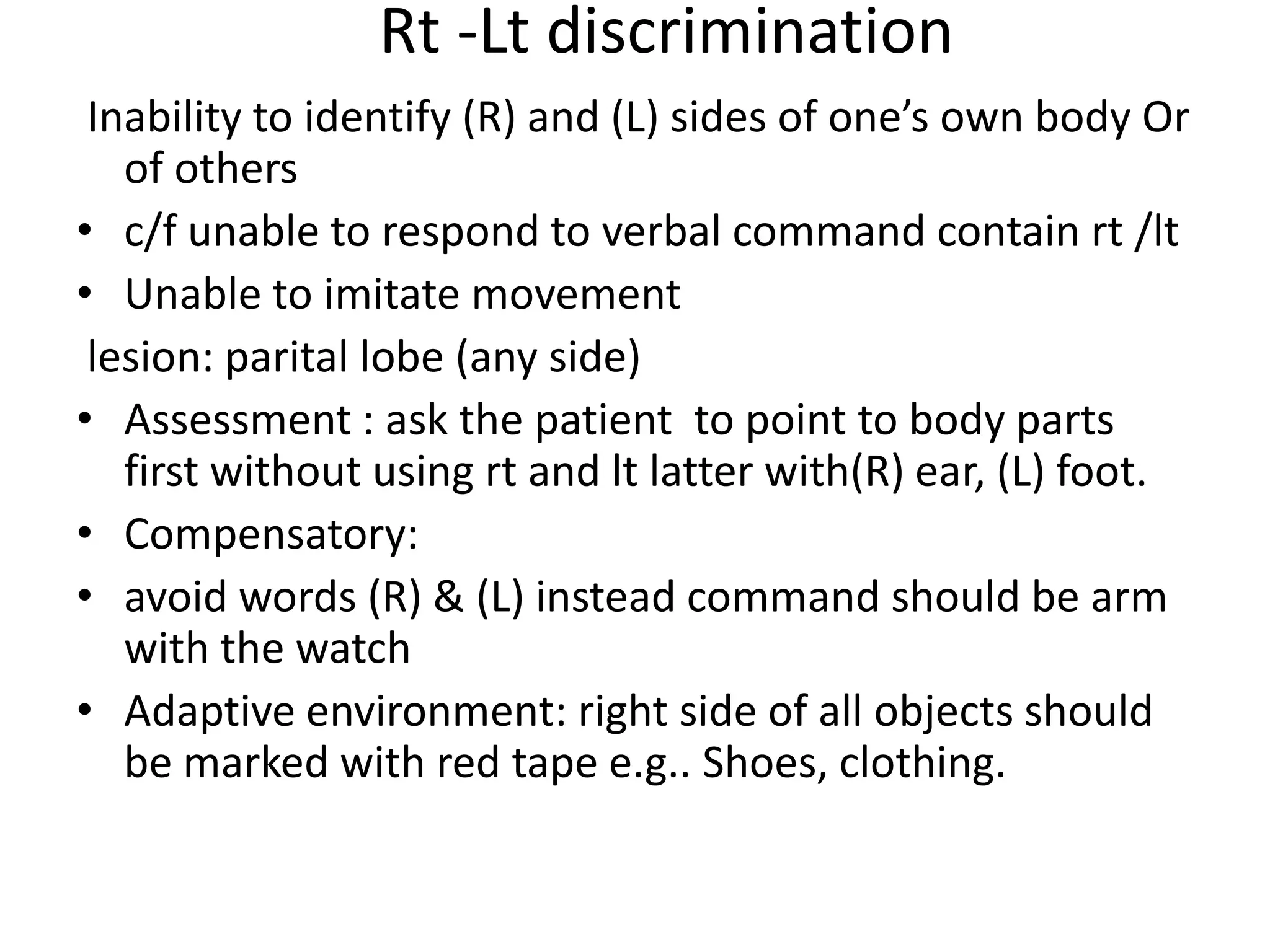
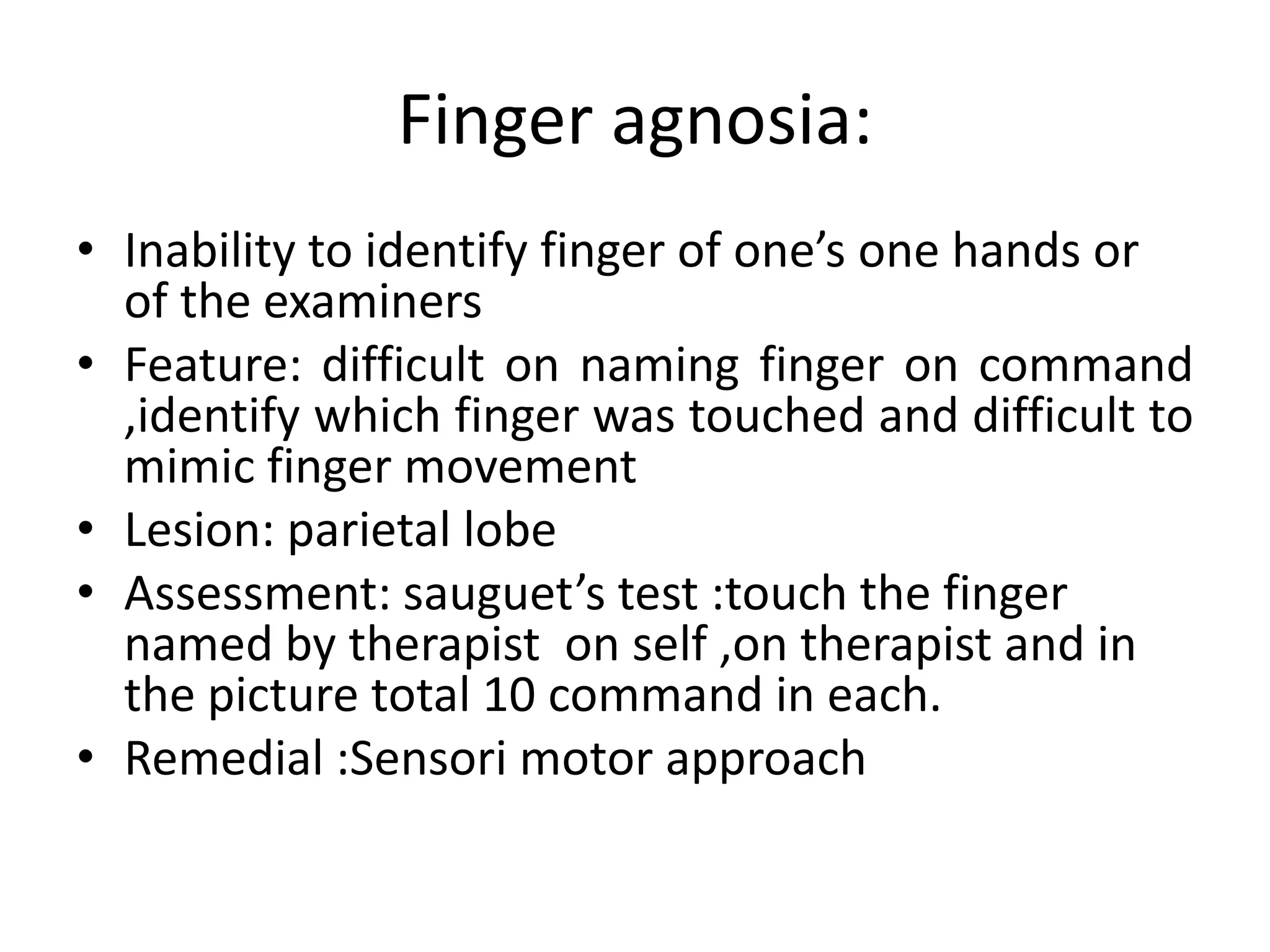
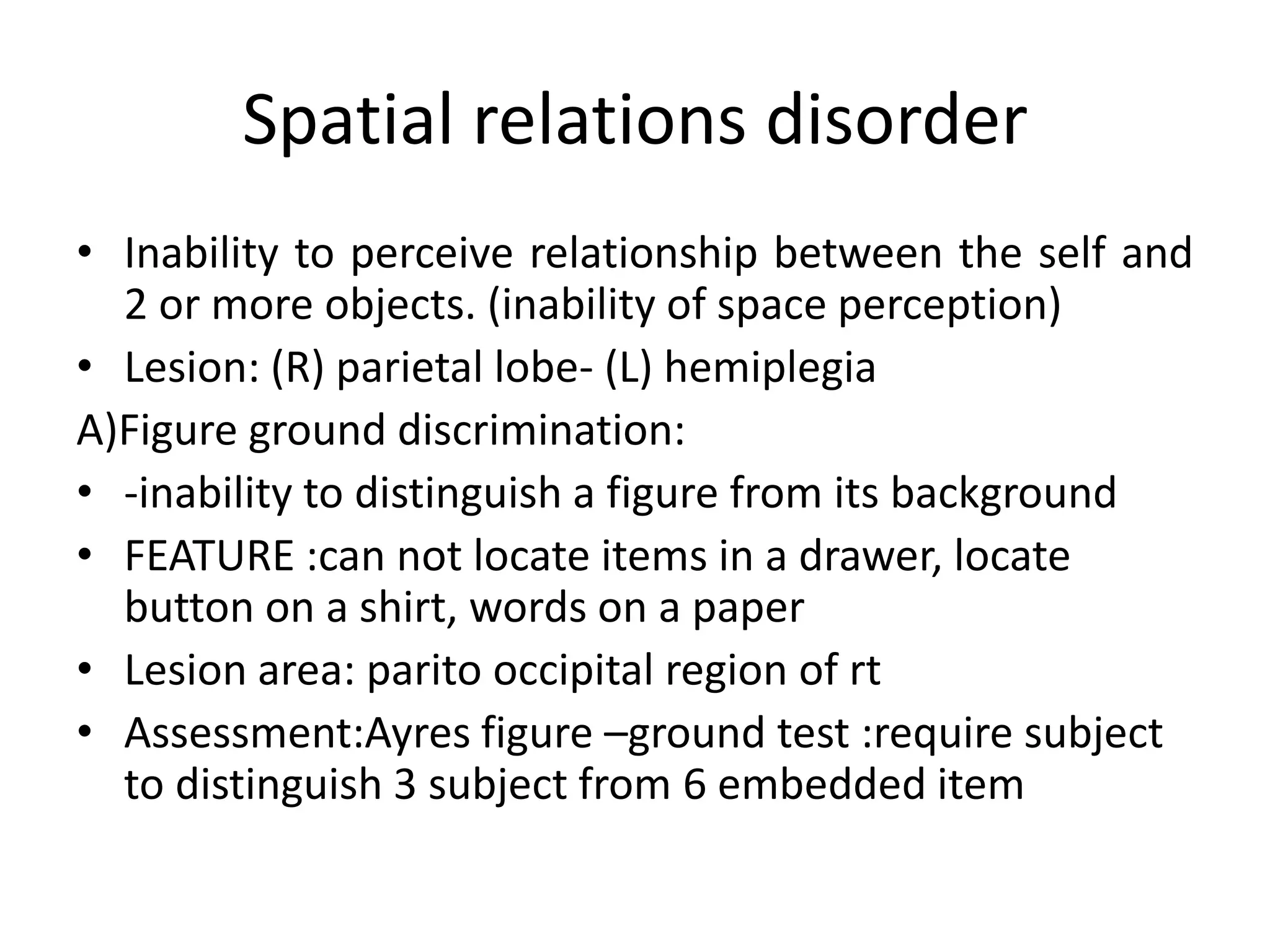
For management, the document discusses five approaches: transfer of training, sensory integrative, neurodevelopmental, functional, and cognitive