This document provides information on assessing the neurological system, including:
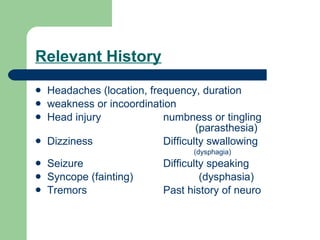
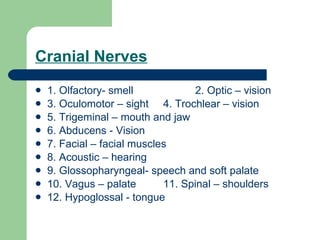
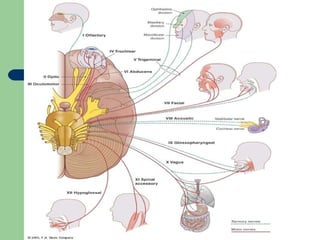
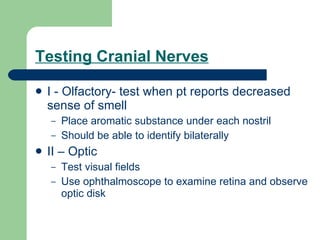
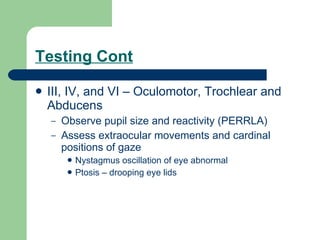
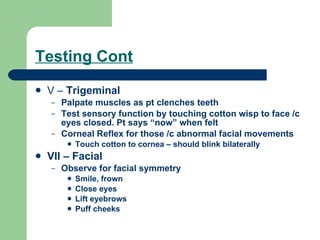
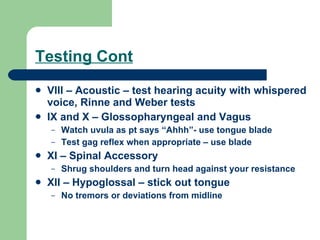
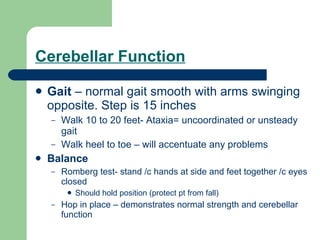
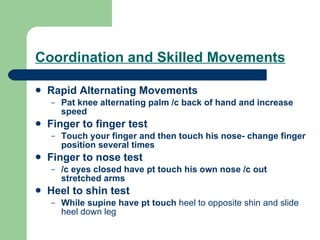
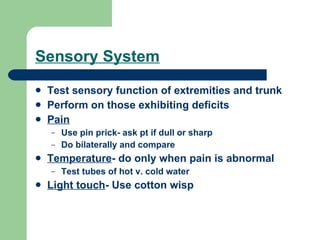
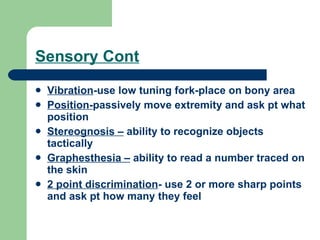
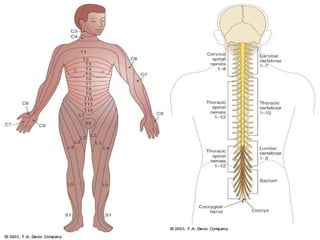
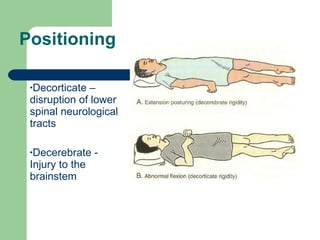
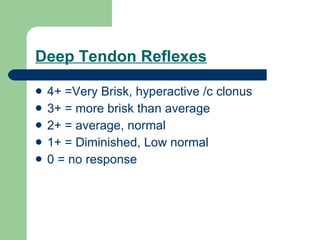
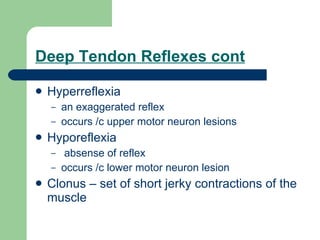
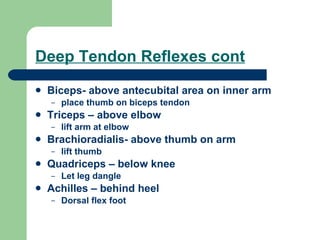
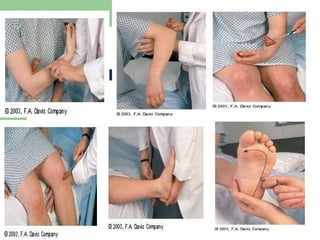
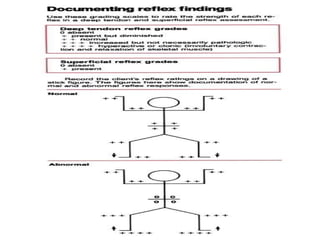
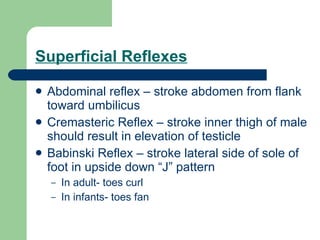
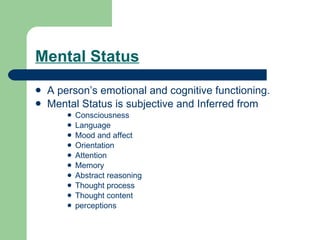
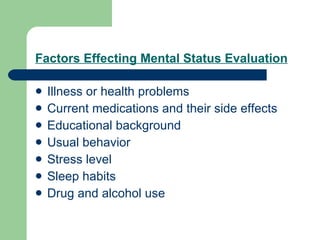
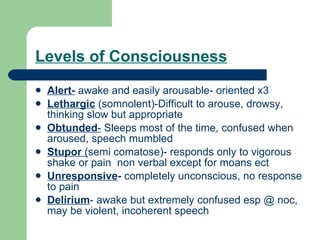
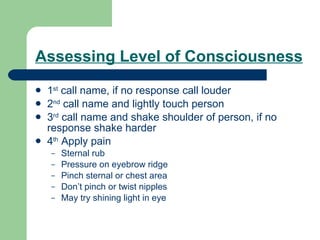
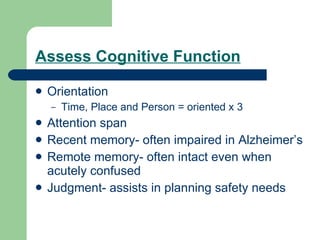
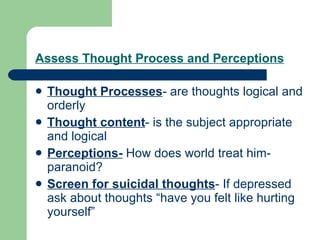
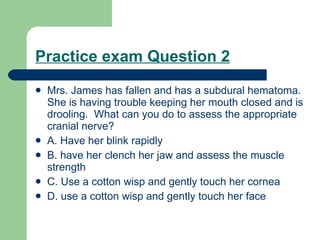
1) It lists relevant history questions and tests various cranial nerves, deep tendon reflexes, sensory function, and mental status.
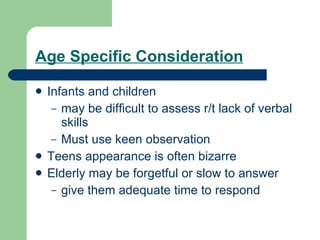
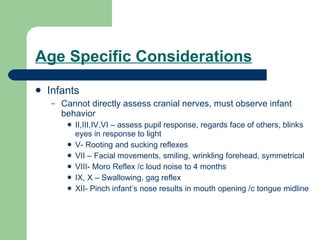
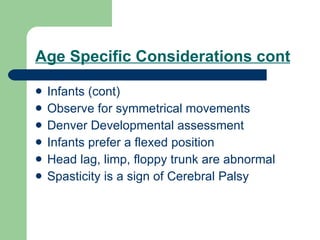
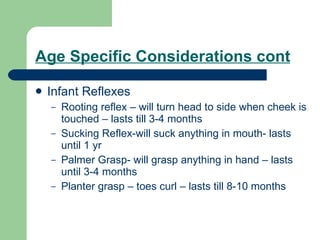
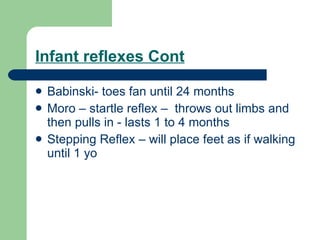
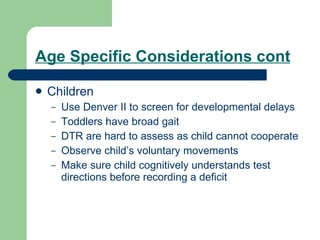
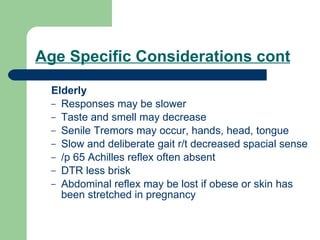
2) It describes age-specific considerations for assessing infants, children, and the elderly.
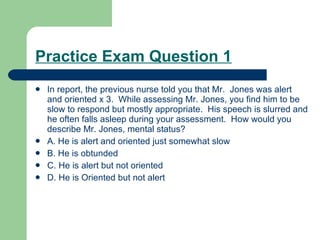
3) It provides examples of practice exam questions and rationales for assessing level of consciousness and identifying the appropriate cranial nerve based on presenting symptoms.