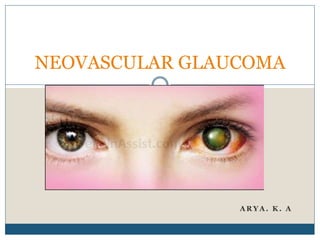
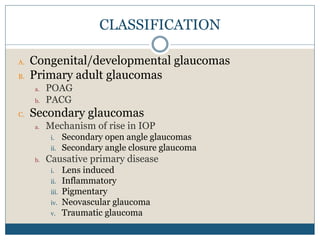
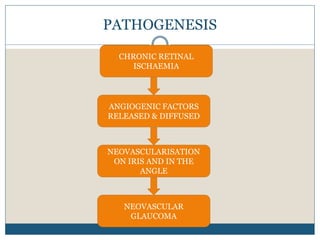
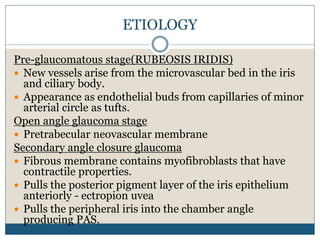
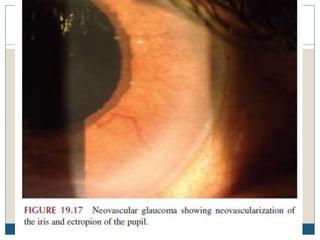
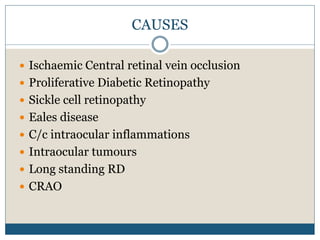
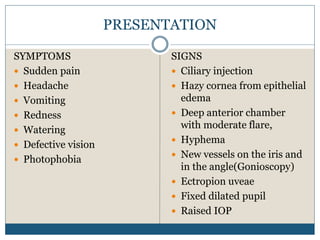
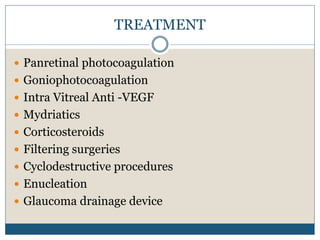
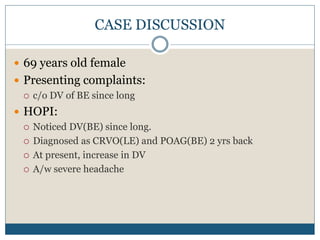
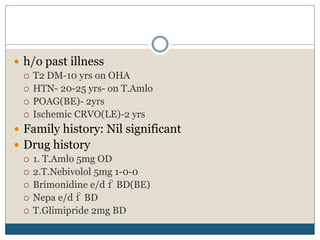
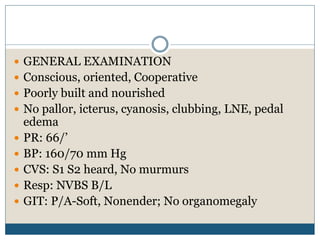
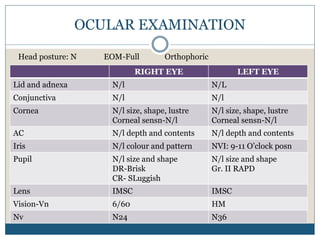
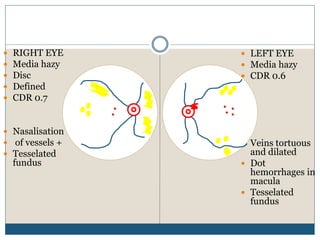
This document discusses neovascular glaucoma (NVG), a type of secondary glaucoma caused by the growth of new blood vessels on the iris and in the anterior chamber angle due to extensive retinal ischemia. NVG is preceded by rubeosis iridis, where new vessels arise from the iris microvasculature. The new vessels can cause open-angle or angle-closure glaucoma by pulling on surrounding structures. Common causes are diabetic retinopathy, central retinal vein occlusion, and other conditions leading to retinal ischemia. Patients present with pain, redness, blurred vision and elevated intraocular pressure. Treatment involves panretinal photocoagulation, anti-VEGF injections, glaucoma medications and