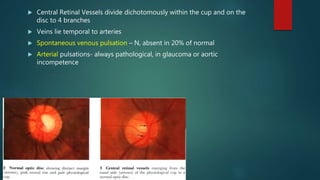
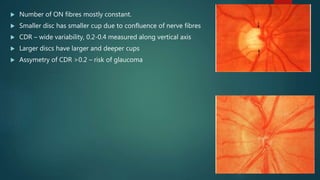
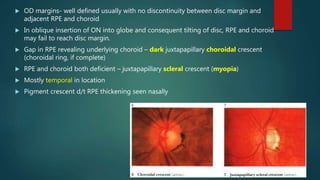
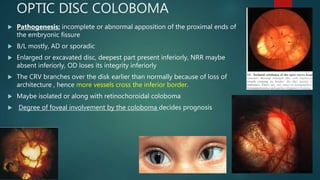
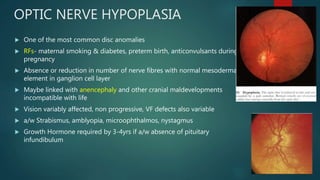
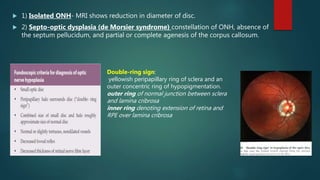
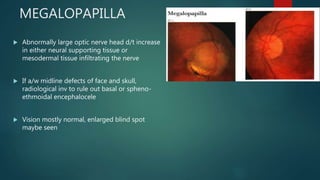
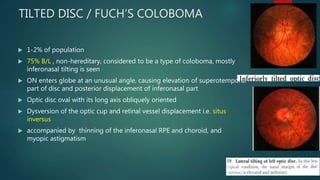
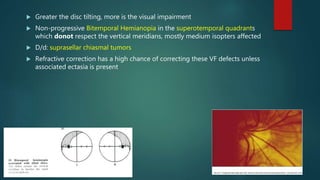
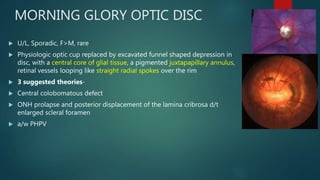
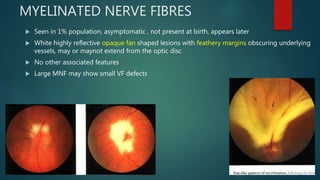
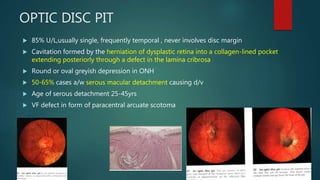
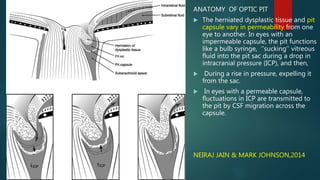
This document provides an overview of congenital optic disc anomalies. It describes the normal optic disc morphology and discusses various anomalies including colobomas, hypoplasia, megalopapilla, tilted discs, morning glory discs, myelinated nerve fibers, and optic pits. For each anomaly, it covers pathogenesis, clinical features, associations, and in some cases, treatment approaches. The key information provided includes a detailed description of the anatomy and histology of the normal optic disc and explanations for how abnormalities during embryonic development can result in different congenital optic disc anomalies.