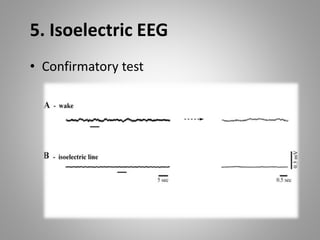
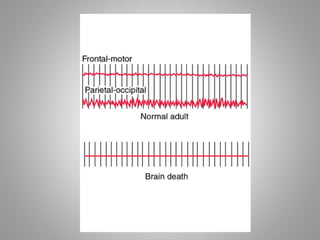
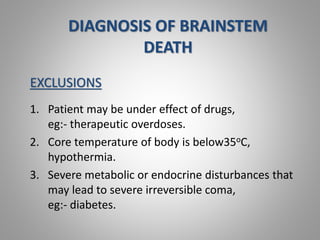
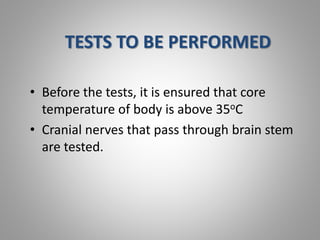
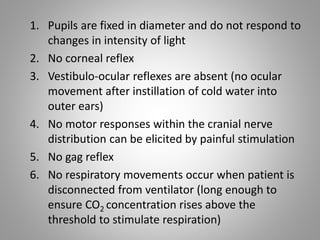
Brain stem death is a type of brain death defined by the absence of brain stem function and reflexes. This results in the permanent loss of consciousness, breathing ability, and other vital functions controlled by the brain stem. Diagnosing brain stem death requires demonstrating the lack of brain stem reflexes, spontaneous breathing, and movement in response to stimuli, along with fixed and dilated pupils and an isoelectric EEG over two examinations 24 hours apart.