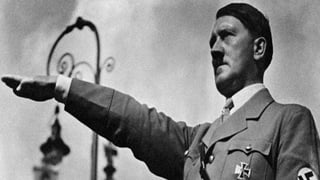
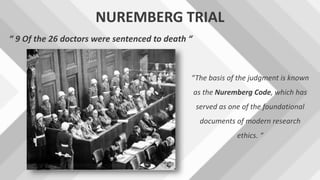
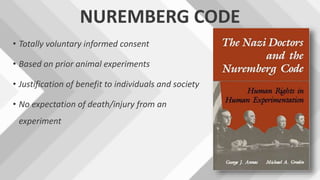
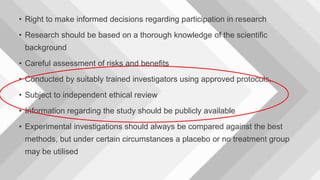
Ethics is concerned with judging what is right and wrong in human conduct. Dental ethics refers to the moral duties of dentists towards patients, colleagues, and society. Key principles of dental ethics include non-maleficence (do no harm), beneficence (do good), respect for patient autonomy and informed consent, justice, truthfulness, and confidentiality. Unethical practices include using unregistered assistants, falsifying records, improper advertising, and undercharging to solicit patients. Historical events like the Nazi experiments, Tuskegee trials, and Declaration of Helsinki established standards to protect research participants through informed consent and review boards. Adherence to an ethical code is important for maintaining trust in the dental profession.



![ETHICAL PRINCIPLES
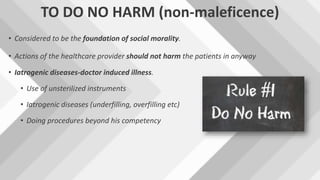
1. to do no harm [ non-maleficence ]
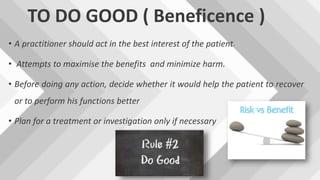
2. to do good [ beneficence ]
3.respect the person
4.Justice
5.veracity or truthfulness
6.confidentiality](https://image.slidesharecdn.com/lectureclasss-170720091936/85/Ethics-in-Dentistry-and-Research-8-320.jpg)

![EHICAL RULES FOR DENTISTS
[given by DCI]
• Duties of dentist towards patients
• Duties of dentists towards one another
• Duties of dentists towards the public](https://image.slidesharecdn.com/lectureclasss-170720091936/85/Ethics-in-Dentistry-and-Research-18-320.jpg)