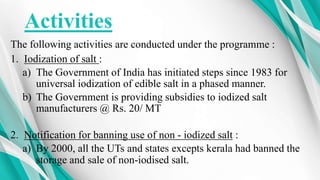
The document summarizes India's National Iodine Deficiency Disorder Control Programme. It outlines that iodine deficiency can cause goiter and other health issues. The program aims to reduce iodine deficiency prevalence below 5% nationally by assessing magnitude, supplying iodized salt, monitoring consumption, and health education. Key strategies include surveys, establishing control cells and labs, training, iodized salt production and distribution, and community awareness. Achievements include significantly reduced goiter rates and increased iodized salt production and monitoring labs in all states. Future plans involve strengthening education in remote areas and the monitoring system to sustain deficiency control.