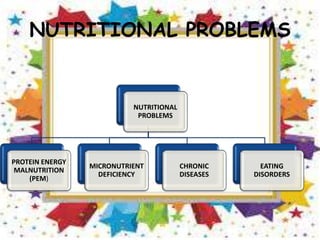
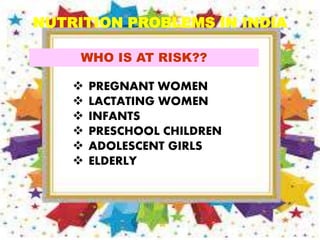
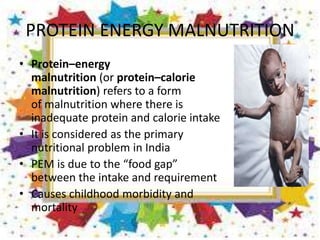
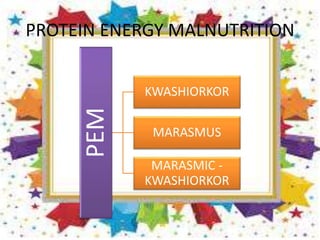
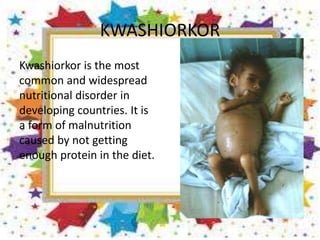
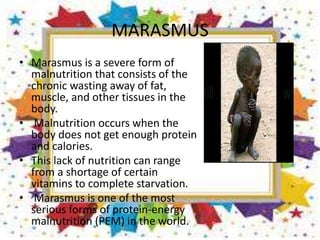
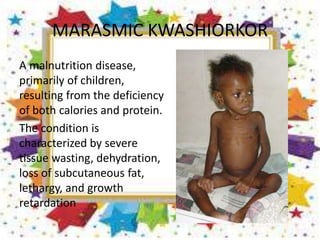
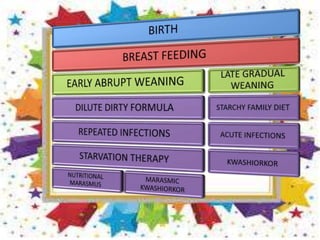
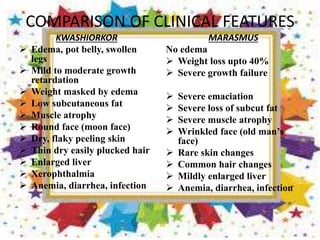
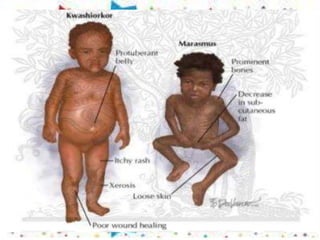
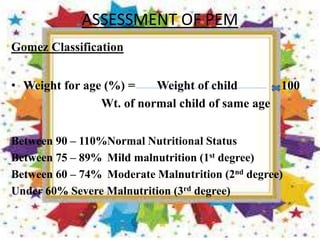
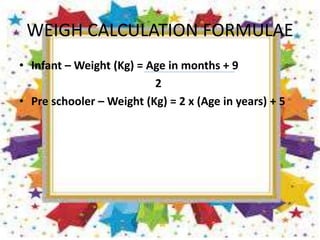
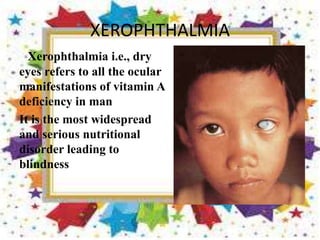
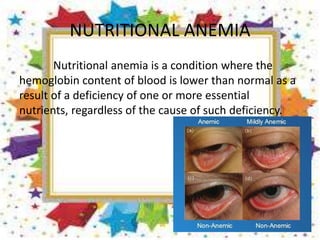
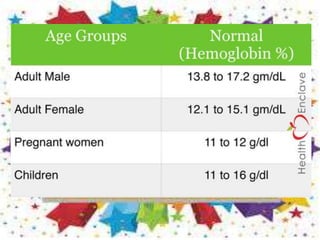
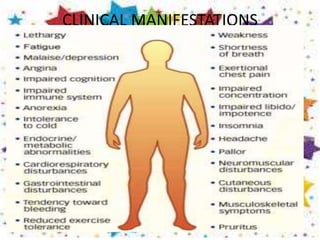
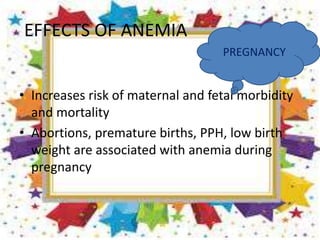
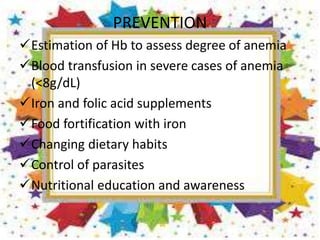
This document discusses various nutritional problems including protein-energy malnutrition, micronutrient deficiencies, and eating disorders. Protein-energy malnutrition manifests as kwashiorkor or marasmus depending on whether there is edema or wasting. Common micronutrient deficiencies in India are vitamin A deficiency which can cause blindness, and anemia. Prevention strategies include breastfeeding, immunization, supplementation, and food fortification. The document provides details on the causes, risk groups, clinical features and management of various nutritional problems.