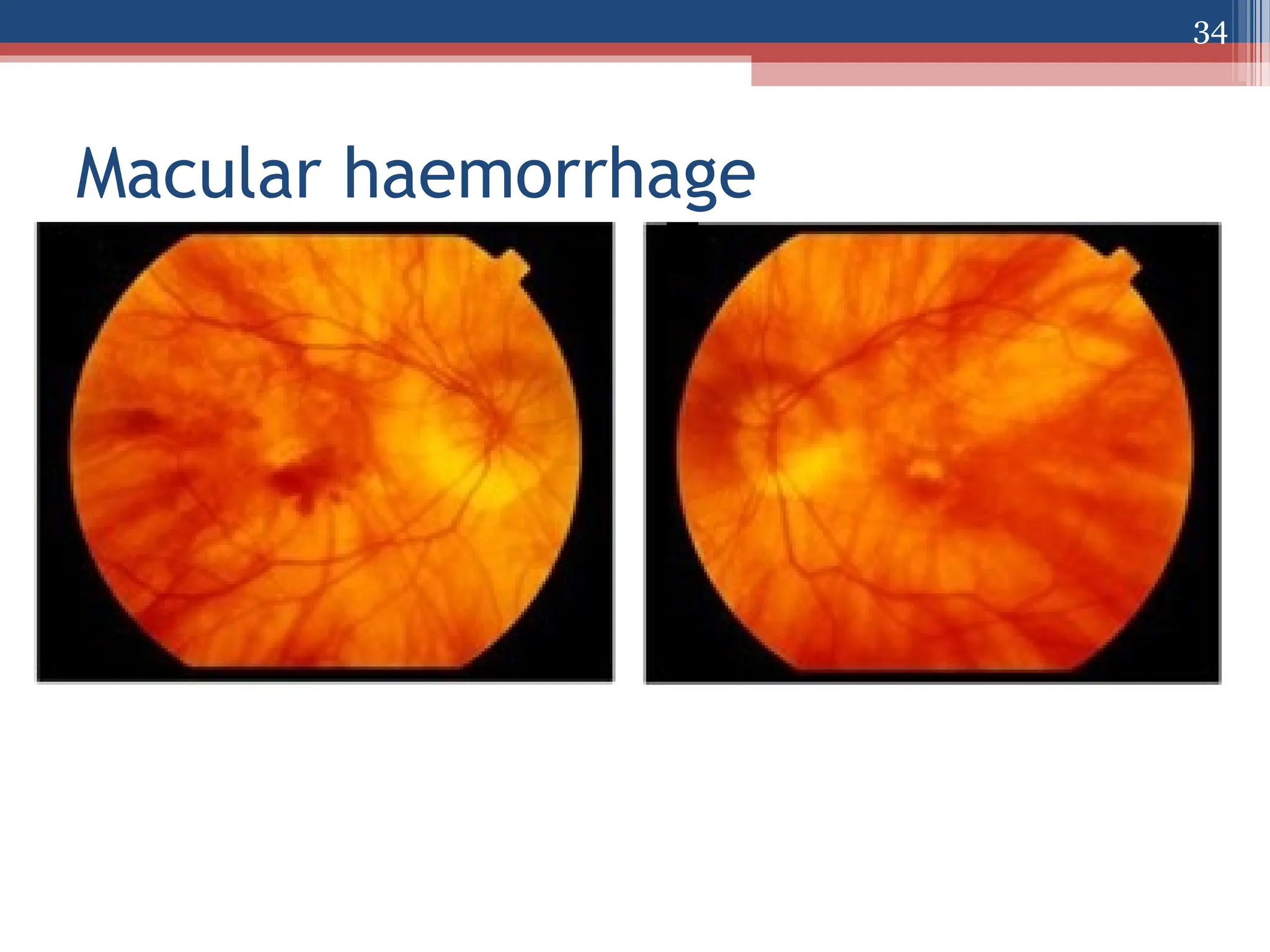
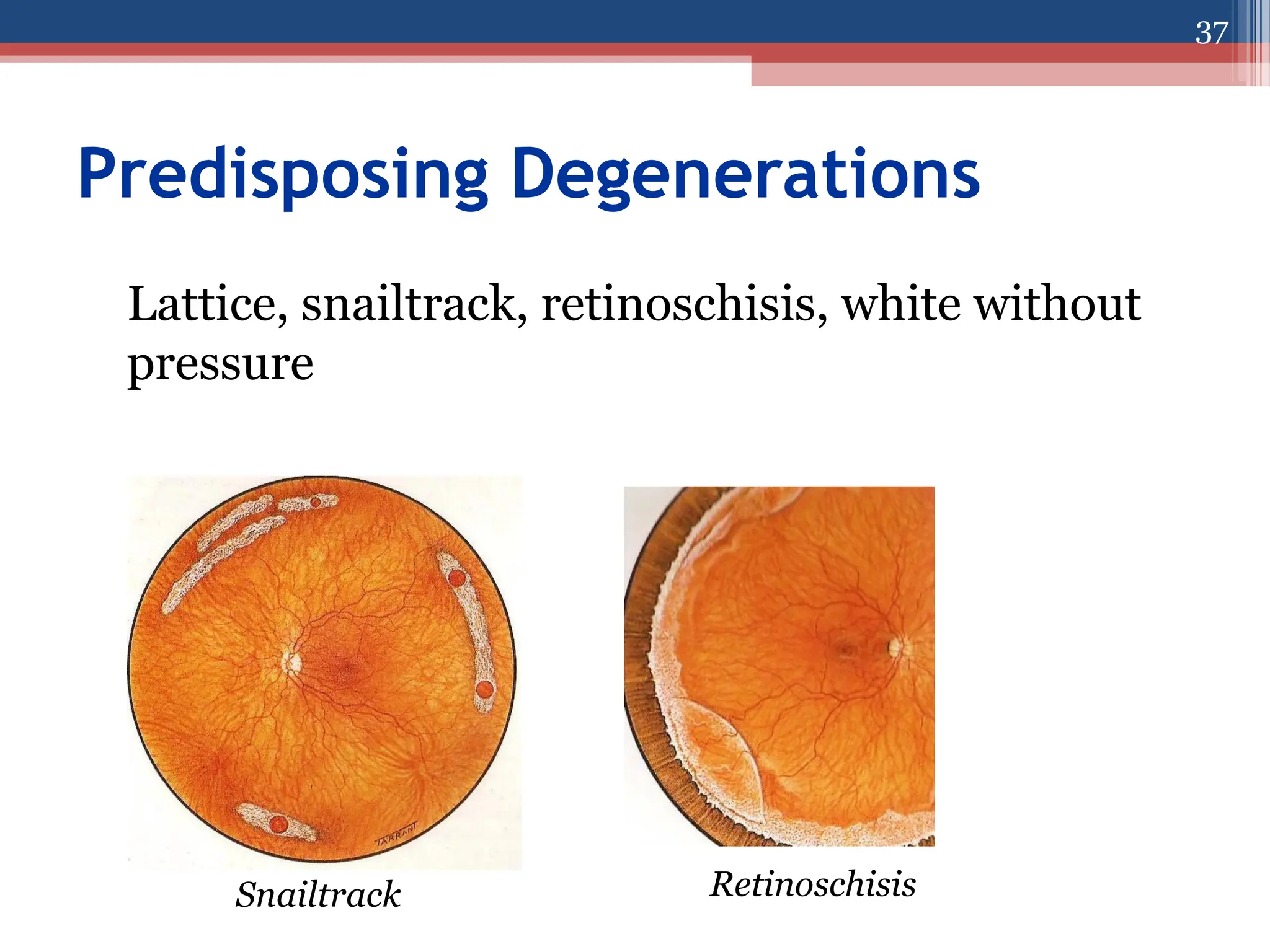
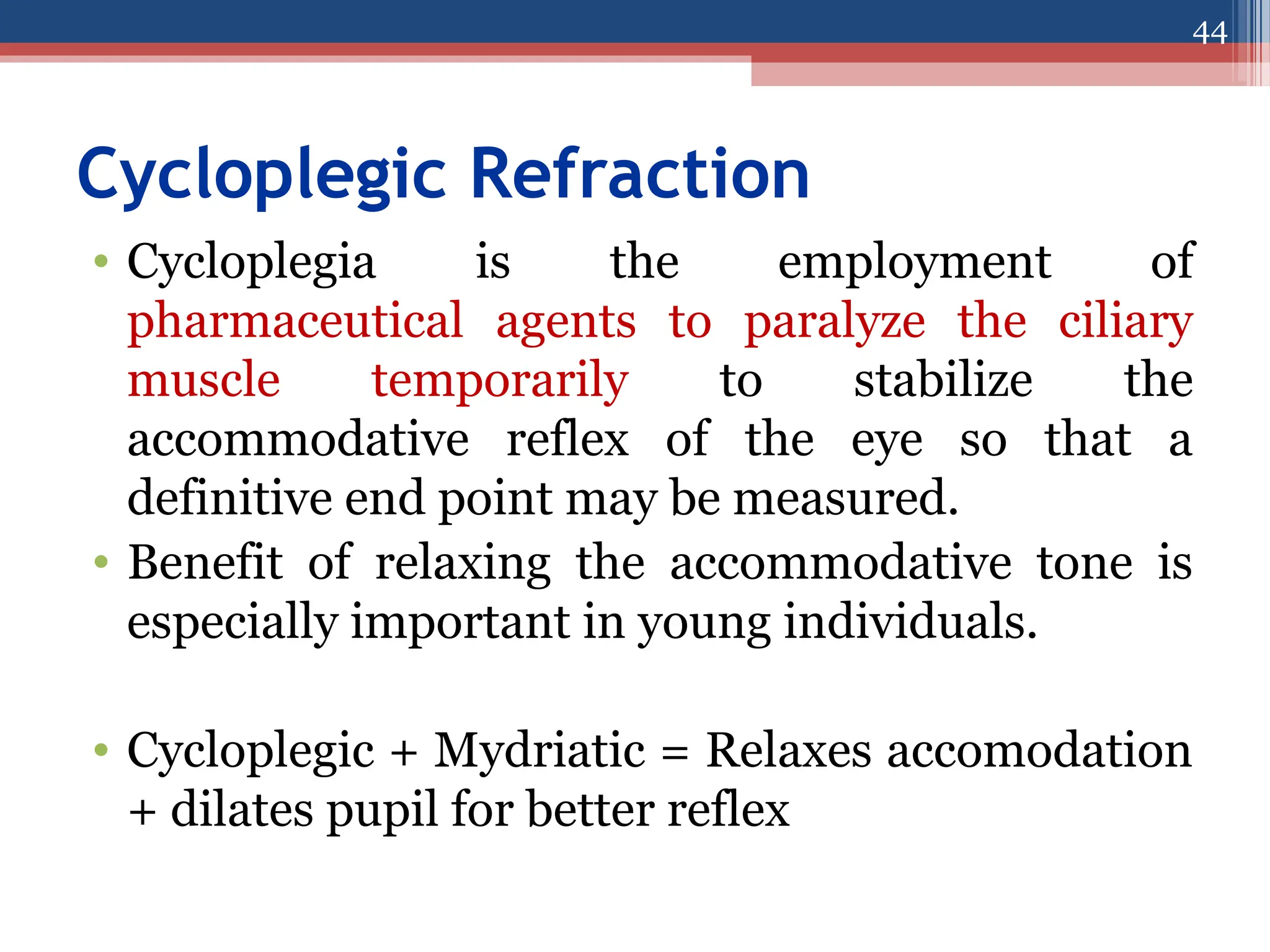
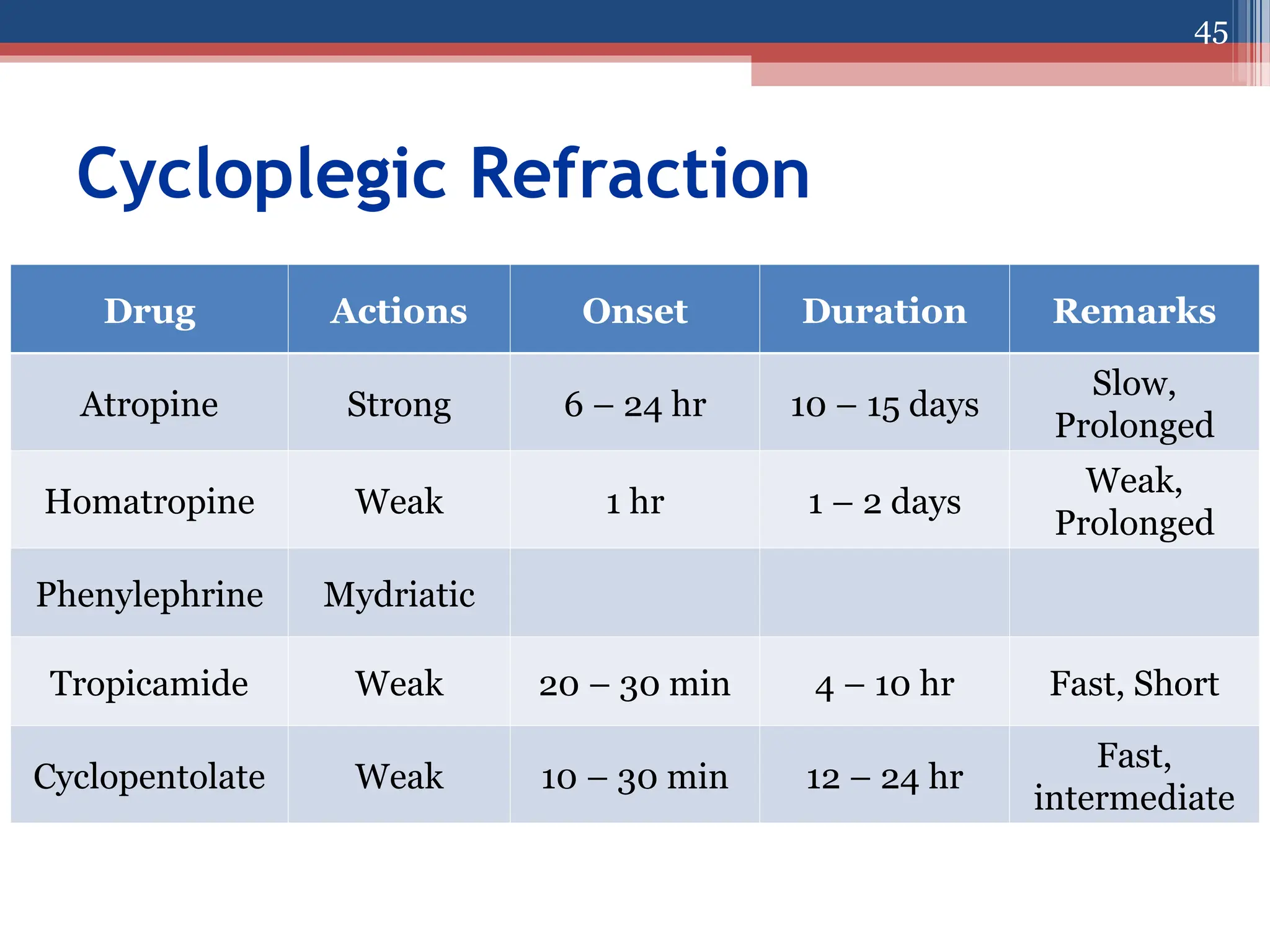
The document focuses on refraction and myopia in ophthalmology, detailing the optical state of the eye and how refractive errors manifest. It explains the different types of myopia, their causes, and associated symptoms and signs. Additionally, it covers treatment options including optical correction, visual hygiene, and refractive surgery.