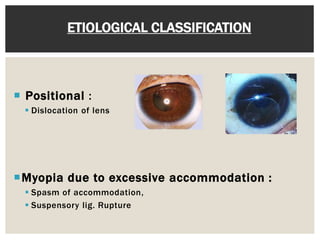
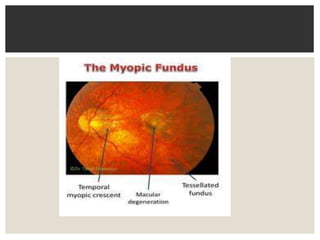
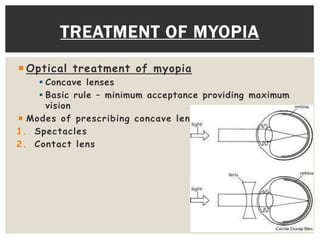
This document discusses myopia (nearsightedness), including its optics, etiological classifications, clinical varieties, and treatment options. Myopia occurs when light rays focus in front of the retina rather than directly on it. It can be axial, curvatural, or positional. Treatment includes optical correction with glasses or contacts, as well as refractive surgeries like LASIK, PRK, clear lens extraction, phakic IOL implantation, intracorneal ring segments, and orthokeratology. More advanced techniques like LASIK and ICLs can correct higher degrees of myopia over -12 diopters.