The document provides an overview of temporomandibular joint disorder (TMJD), including its history, definition, symptoms, diagnosis, and treatment options. Some key points:
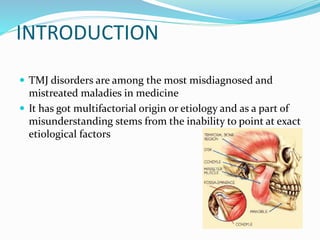
- TMJD has multiple potential causes and is often misdiagnosed due to various etiological factors. It involves pain in the preauricular region and muscles of mastication.
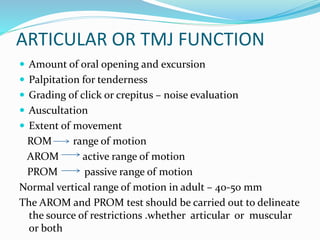
- Diagnosis involves examining the jaw joint, muscles, teeth, and cervical spine. Imaging like panoramic x-rays may also be used.
- Treatment includes medications like NSAIDs, muscle relaxants, and antidepressants. Physical therapies include heat/ultrasound, exercises, and stress management techniques. Occlusal splints are


![HISTORY
Costen[1934]-occlusal etiology in TMJ pain
Schwartz[1956]-term TMJ pain dysfunction
syndrome
Laskin[1969]-provocative paper on MPDS
Mackenzie and Banks and Toller and
Poswillo[1975]-diagnosis & treatment of intrinsic
joint disorders](https://image.slidesharecdn.com/myofacialpaindysfunctionsyndrome-221221062809-adb75c02/85/MYOFACIAL-PAIN-DYSFUNCTION-SYNDROME-pptx-4-320.jpg)

![PATHOPHYSIOLOGY[ETIOLOGY ]
Extrinsic factors
-Trauma
-Occlusal
disharmony
-Habits
-Psychological
Intrinsic factors
-Internal
derangement of
TMJ
-Anterior locking of
disc
-Meniscal
displacement due to
trauma](https://image.slidesharecdn.com/myofacialpaindysfunctionsyndrome-221221062809-adb75c02/85/MYOFACIAL-PAIN-DYSFUNCTION-SYNDROME-pptx-6-320.jpg)














![NSAIDS
• To reduce inflammation and to provide pain relief
• 14 -21 days
MUSCLE
RELAXANT
• Recommended only for short duration
• Diazepam[2-5mg] ,cyclobenzapine 10mg at bedtime
[10 days ]
ETHYL
CHLORIDE
SPRAY
• or intramuscular injection
• 2% lignocaine or 0.05 % bupivacaine can be used](https://image.slidesharecdn.com/myofacialpaindysfunctionsyndrome-221221062809-adb75c02/85/MYOFACIAL-PAIN-DYSFUNCTION-SYNDROME-pptx-23-320.jpg)



![ STABILIZATION SPLINT
Reduces the load on the retrodiskal area and thereby
reduce the pain
Used to eliminate occlusal interference with bruxism
12-18 hours use is advocated up to 4-6 months
Follow up is done until the occlusion is stabilized and
muscles are free of tenderness
• RELAXATION SPLINT
Used for disengagement of teeth and only for short periods
[up to 4 weeks ]
Fabricated over the maxillary teeth and a platform is added
to disengage mandibular anterior](https://image.slidesharecdn.com/myofacialpaindysfunctionsyndrome-221221062809-adb75c02/85/MYOFACIAL-PAIN-DYSFUNCTION-SYNDROME-pptx-27-320.jpg)
![TMJ ARTHROCENTESIS
Simple treatment for limited mouth opening accompanied by
severe pain
OBJECTIVE
Improve the disk mobility
Eliminate joint inflammation
Eliminate pain
Early physiotherapy
Remove the resistance to condyle translation .return to
normal function
• INDICATION
All patients who had proved refractory to conservative
treatment [medication ,bite appliances ,physiotherapy and
manipulation of joint ]](https://image.slidesharecdn.com/myofacialpaindysfunctionsyndrome-221221062809-adb75c02/85/MYOFACIAL-PAIN-DYSFUNCTION-SYNDROME-pptx-28-320.jpg)







![REFERENCE
Textbook of oral and maxillofacial surgery –Neelima Anil
Malik[3rd edition ]
Textbook of oral and maxillofacial surgery –
Chitra Chakravarthy (2nd edition )](https://image.slidesharecdn.com/myofacialpaindysfunctionsyndrome-221221062809-adb75c02/85/MYOFACIAL-PAIN-DYSFUNCTION-SYNDROME-pptx-36-320.jpg)
