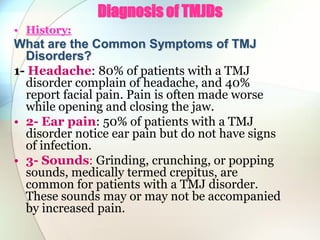
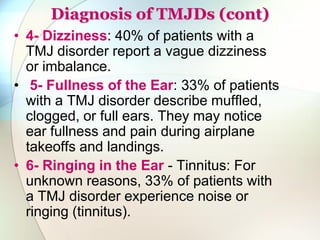
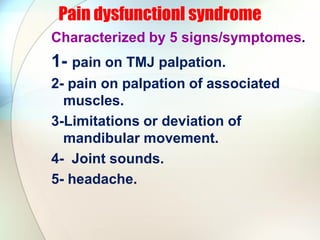
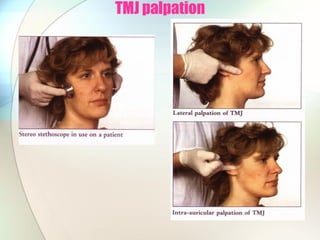
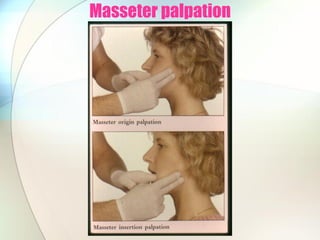
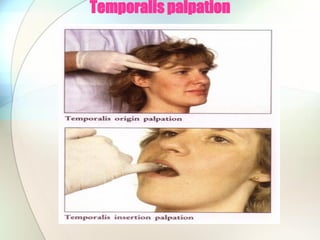
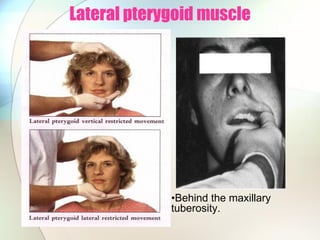
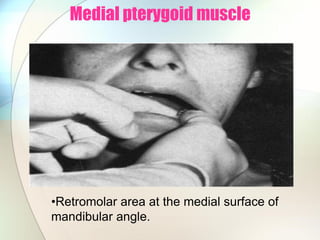
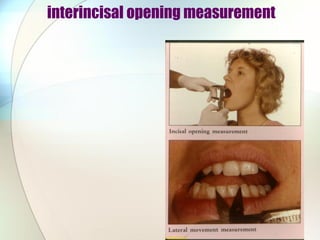
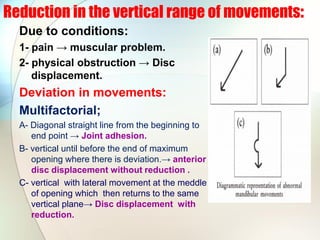
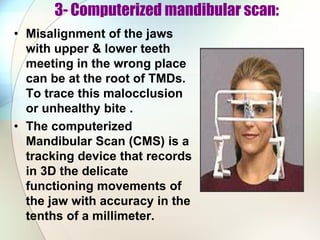
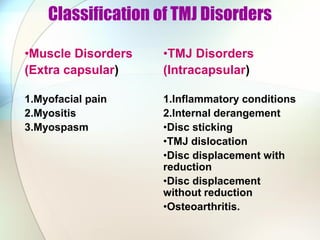
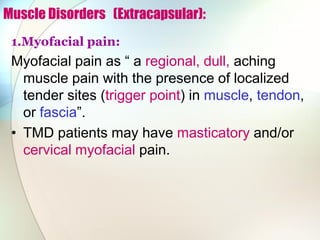
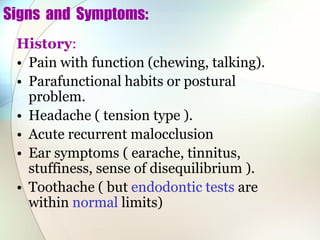
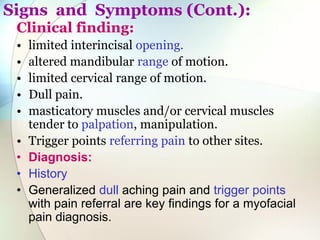
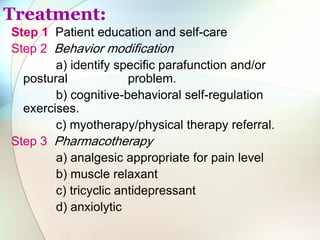
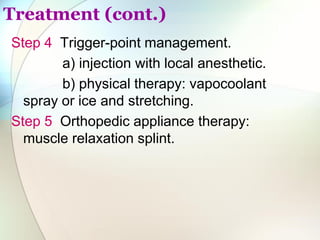
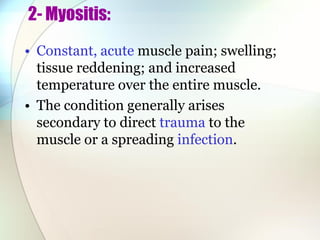
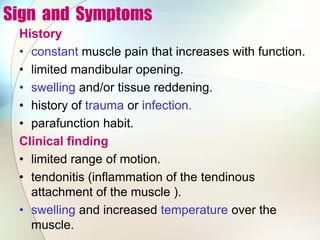
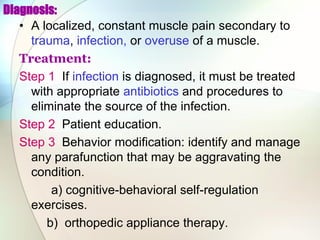
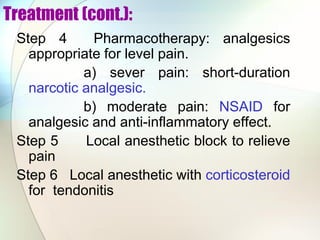
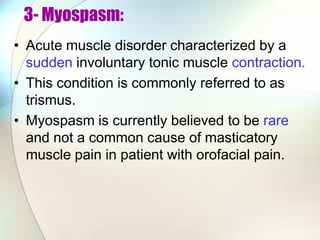
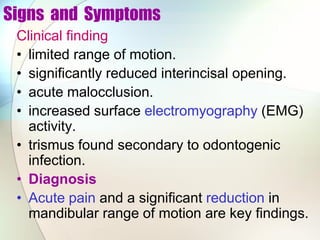
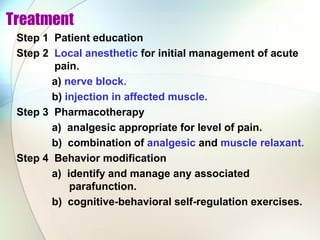
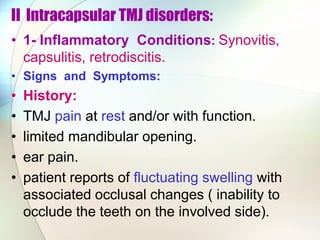
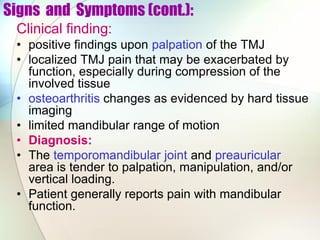
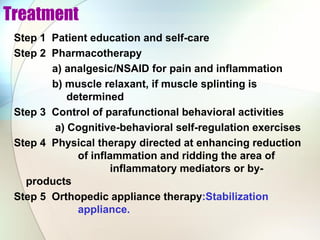
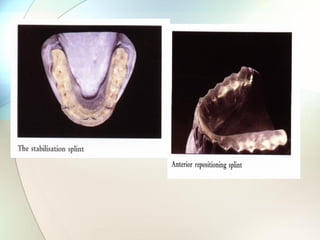
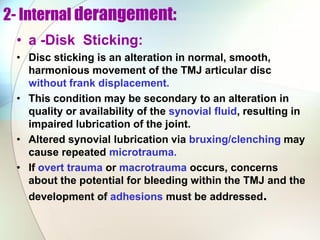
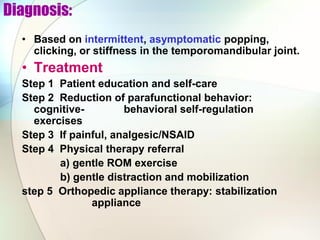
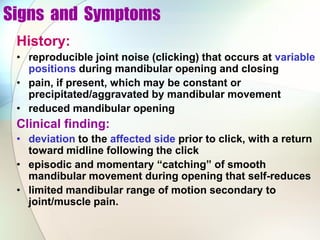
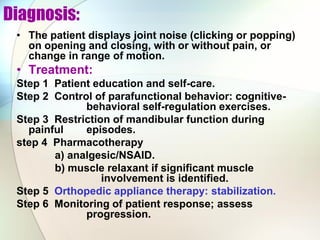
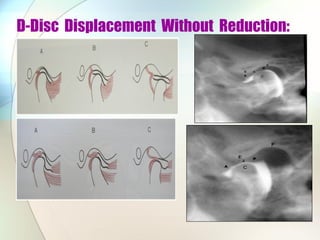
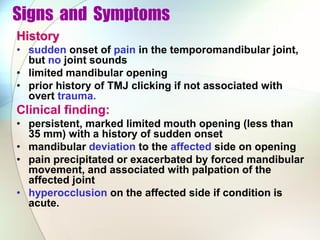
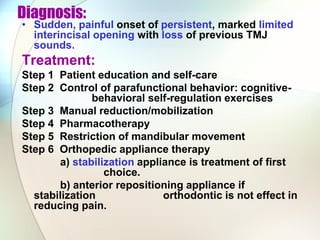
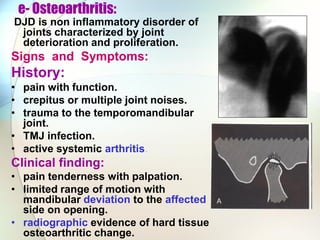
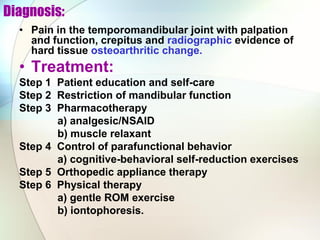
This document discusses diagnosis and treatment of temporomandibular joint disorders (TMJDs). It describes common symptoms such as headaches, ear pain, sounds from the joint, and limited jaw movement. Diagnosis involves patient history, clinical examination including palpation of the jaw and muscles, and sometimes imaging tests. TMJDs can be classified as muscle disorders, joint disorders, or a combination. Treatment depends on the specific disorder but may include education, behavior modification, physical therapy, medications, and dental appliances.