This document provides information on the temporomandibular joint (TMJ), including its definition, structure, diagnosis, and treatment of TMJ disorders. Some key points:
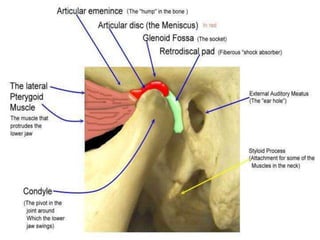
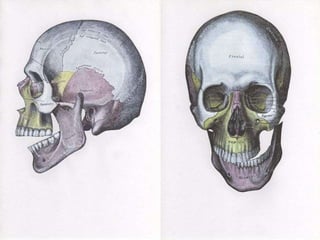
- The TMJ is formed by the temporal bone and mandible, allowing hinging and sliding movements. It contains an articular disc that helps distribute forces.
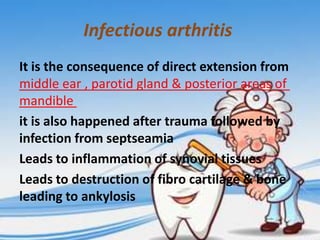
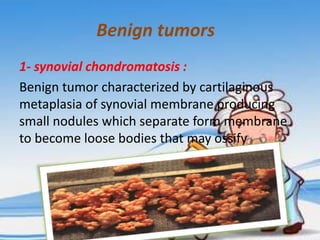
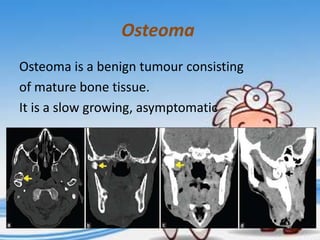
- Common TMJ disorders include myofascial pain dysfunction syndrome, osteoarthritis, dislocations, and internal derangements (abnormal disc positioning).
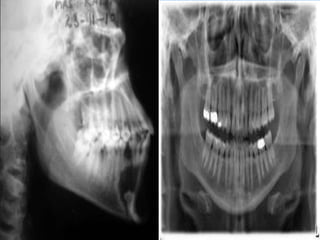
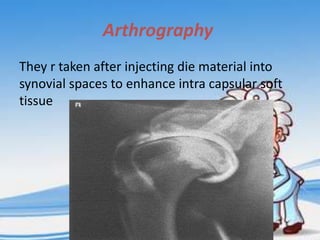
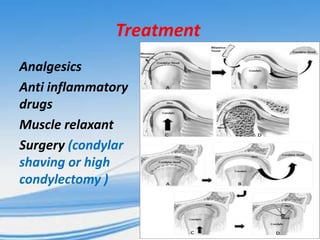
- Diagnosis involves history, examination, and imaging like x-rays, CT, MRI. Treatment depends on the disorder but may include splint therapy, exercises, injections, or surgery.