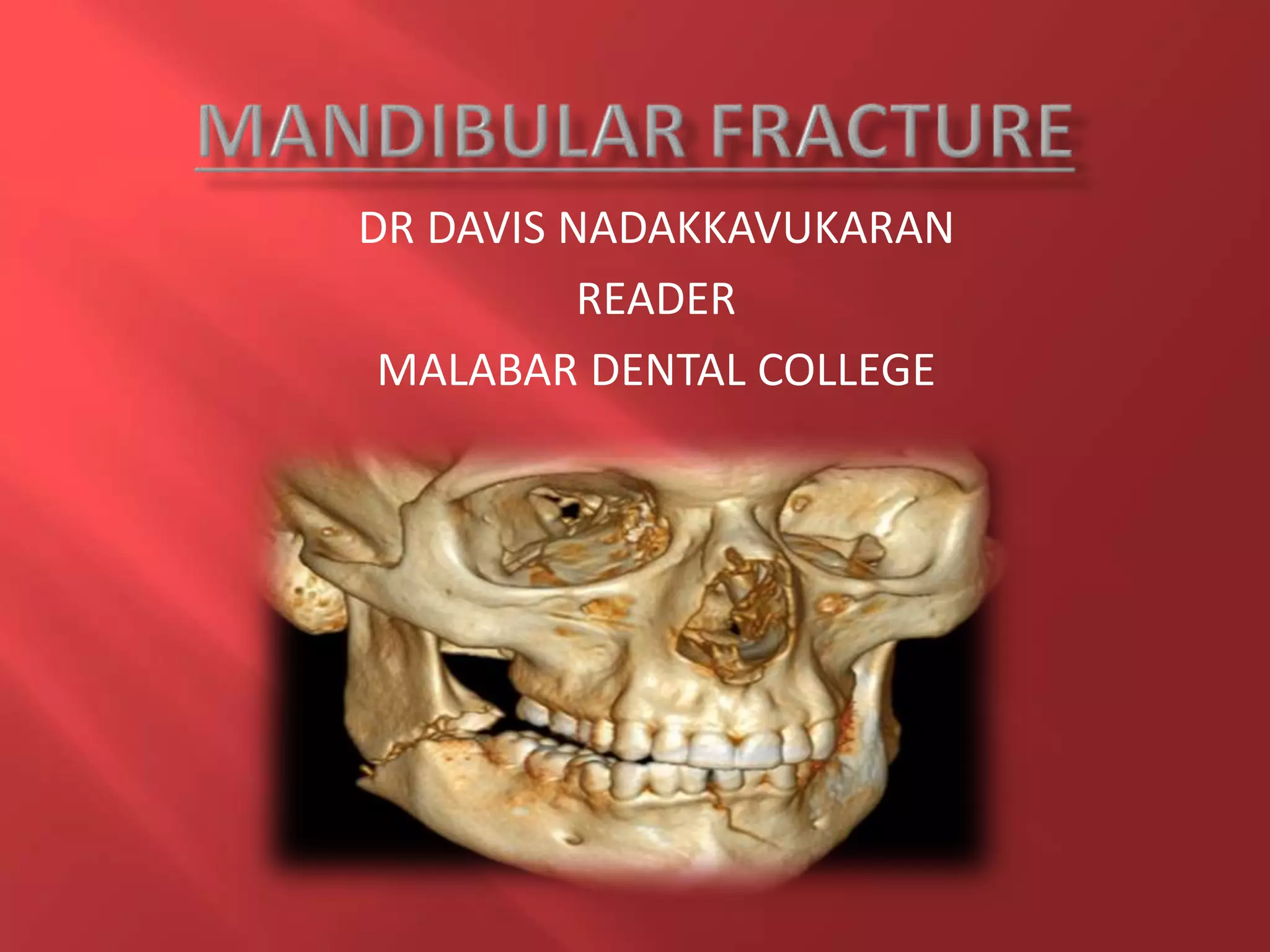
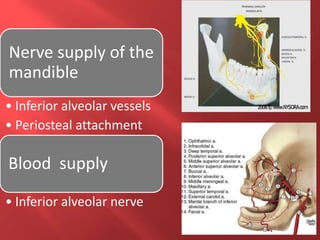
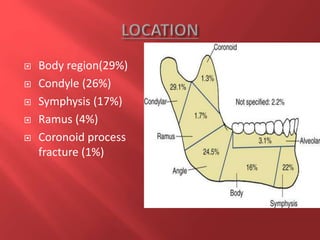
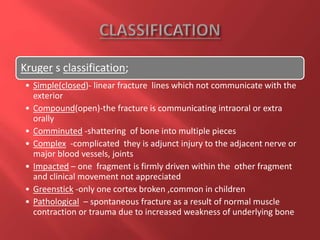
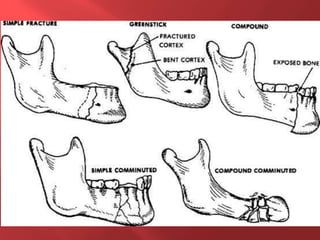
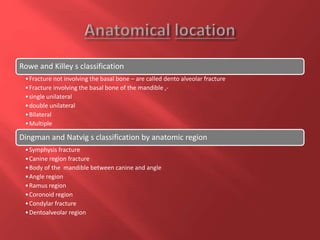
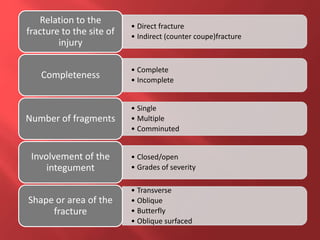
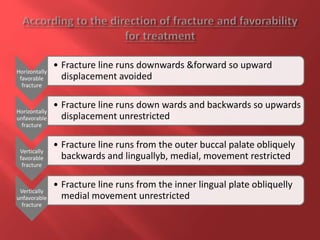
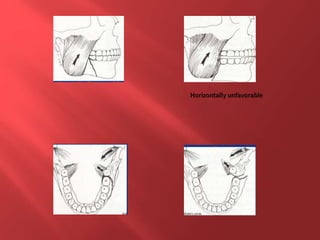
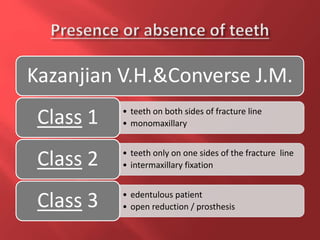
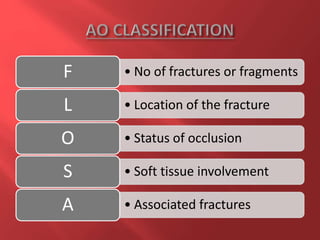
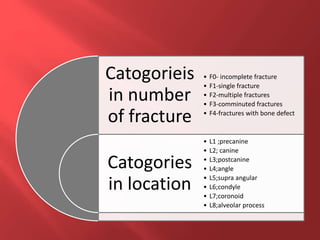
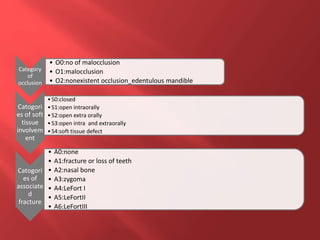
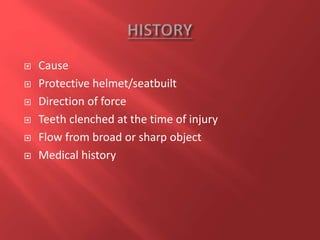
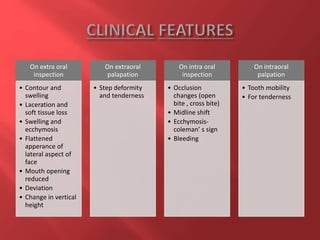
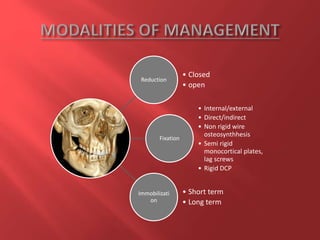
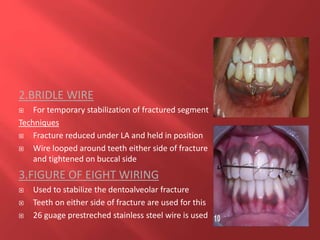
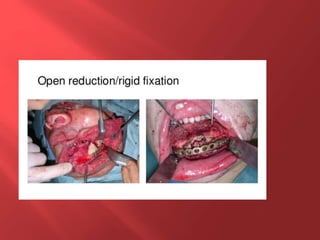
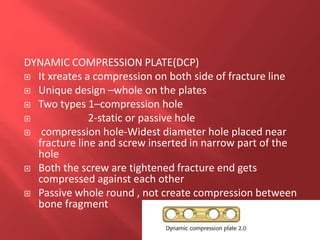
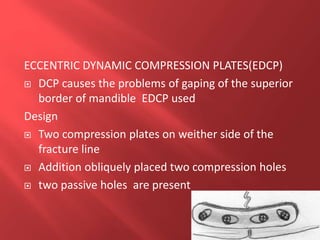
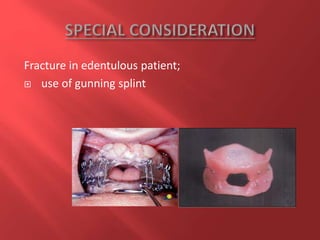
This document discusses the anatomy, classification, diagnosis, and management of mandibular fractures. It begins with the anatomy of the mandible and then covers the common causes and locations of mandibular fractures. It describes several classification systems for mandibular fractures. Diagnosis involves clinical examination, radiographs, and sometimes CT imaging. Management depends on factors like fracture location and complexity, and can involve closed or open reduction with fixation methods like plates, screws, or wiring. The goal is to restore proper occlusion and fixation while avoiding complications.