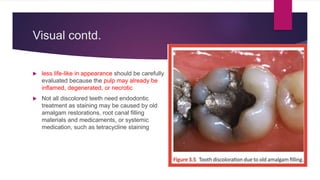
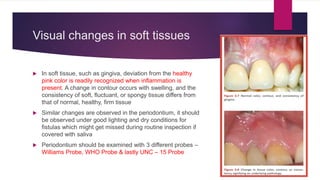
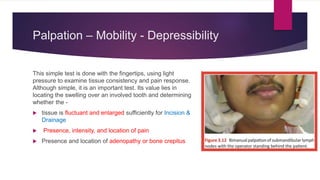
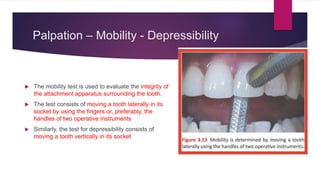
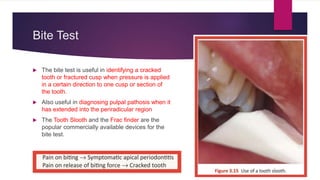
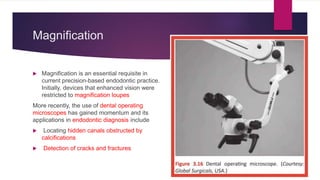
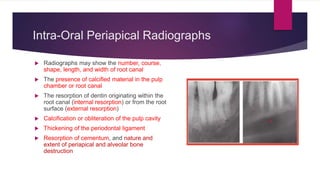
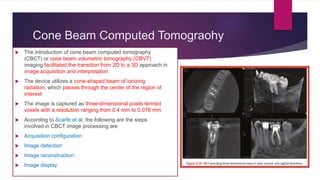
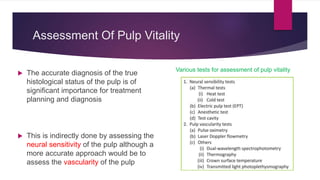
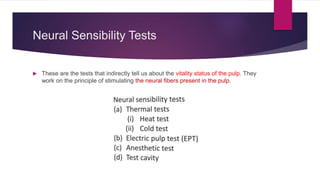
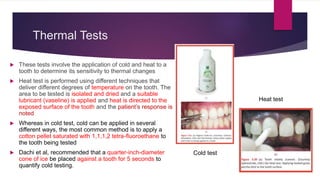
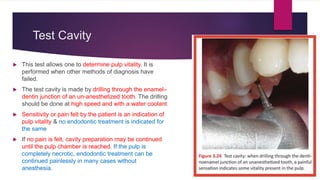
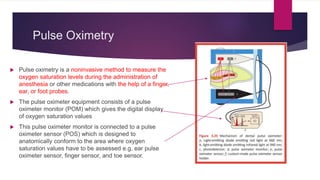
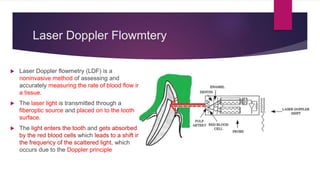
The document discusses diagnostic aids in endodontics, focusing on the processes of clinical examination and diagnosis, including various symptoms and tests used to identify dental issues. It highlights the importance of understanding both subjective and objective symptoms and describes diagnostic tests such as radiography, pulp vitality testing, and the use of technology like cone beam computed tomography. The information is primarily sourced from Grossman's Endodontics, emphasizing the necessity of thorough assessment to guide treatment planning.