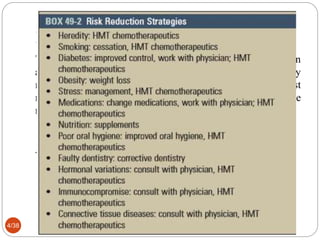
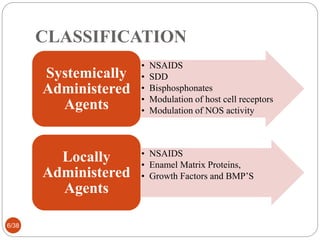
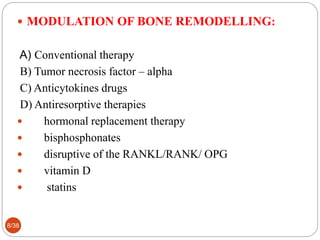
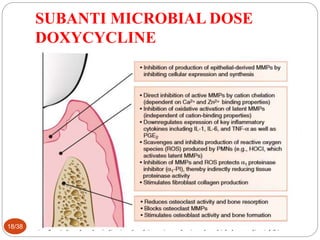
The document discusses host modulation therapy (HMT) as a treatment for periodontitis, emphasizing its role in modifying the host's inflammatory response to promote tissue regeneration and reduce disease progression. It details various host modulating agents, including NSAIDs, bisphosphonates, and new emerging treatments like azithromycin, alongside their mechanisms and indications. The conclusion reiterates that while plaque bacteria are necessary for periodontitis, successful treatment requires a susceptible host and effective modulation of the host's immune response.